From distance learning to social distancing, UMHS students are coping with the COVID-19 pandemic as many have returned home and are finishing up the semester online
The UMHS Endeavour spoke to Nichole Cumby, PhD., UMHS Assistant Professor of Microbiology, about the COVID-19 pandemic and what UMHS students should know about the new distance learning platform, from how students can engage with professors and enhance their medical education to the opportunities it provides for Caribbean medical schools. Dr. Cumby also discussed COVID-19 and numerous aspects students and the public must know to stay healthy and protect others.
 UMHS started using Blue Button & Zoom distance learning platforms in March 2020. Photo: Deposit Photos.
UMHS started using Blue Button & Zoom distance learning platforms in March 2020. Photo: Deposit Photos.
New Distance Learning Platforms at UMHS
UMHS moved to a distance learning format due to the COVID-19 pandemic earlier this month. The school remains open using the Big Blue Button and Zoom distance learning platforms.
Dr. Nichole Cumby talked about what current and incoming UMHS students must know about the new distance learning platform. How does it work and is it effective?
“When we were initially making the move to distance, I had some concerns about how easy it would be to continue to engage with students in the classroom,” Dr. Cumby said. “Good teaching depends on engagement. However, I have found that certain features of our online platforms actually enhance student engagement. I can ask questions and create an audience poll to see how well a class is understanding a current topic. Students can easily ask questions in class via the text chat feature and I find we get way more back and forth discussions going this way – between myself and the students with each other. In many ways it is highly interactive. Students can really take advantage of the tools in the lecture to interact with their professors, ask questions and learn.”
What are some challenges in getting something working so quickly?
“As with any new technology, some of the biggest challenges were becoming familiar with how to use the software and adapting previously offline lectures to the online format while maintaining quality. Fortunately, fellow faculty familiar with the software like Dr. Peter Lee made videos to train both faculty and students in its use which really helped us get ready. Dr. Young volunteered to help teach interested faculty how to use certain platforms. Additionally, ensuring all faculty had the required equipment (e.g. microphones, etc.) to deliver online features was also a difficulty we had to overcome quickly in order to get lectures resumed in a timely fashion.”
What opportunities does distance learning provide for Caribbean medical schools?
“One of the powerful things about online learning is that geography is no longer a barrier to education,” Dr. Cumby said. “This gives students way more flexibility than previously. Limitations that might have previously created barriers to education like location and time can be removed. Caribbean medical schools always have a chance to get disrupted by hurricane season, but with a solid distance platform in place, the impact to a student’s learning will be minimal in the event of any sort of situation like this. Additionally, it is a great opportunity not only to add in some modern learning tools but also to master the latest technology which is becoming more and more relevant and helpful in every career path including medicine. Finally, the biggest advantage is the potential for continuing education, collaboration and connectivity.”
Distance learning has a positive benefit for 5th semester clinical students.
“When students head out to Maine, they can still easily contact instructors on St. Kitts for ongoing support,” Dr. Cumby said. “They can even attend online lectures for topics that have given them trouble previously from anywhere. Students will be able to direct their own learning themselves. They can decide what topics give them the biggest issues and sit in on extra lectures at any time, from anywhere. Once they have matched into various hospitals, they can also choose to sit in on updated lectures too, to stay up to date on any changes and advances in the field. It is powerful to be able to remain connecting and learning, anytime from anywhere. This technology really lets us break down barriers in the education process.”
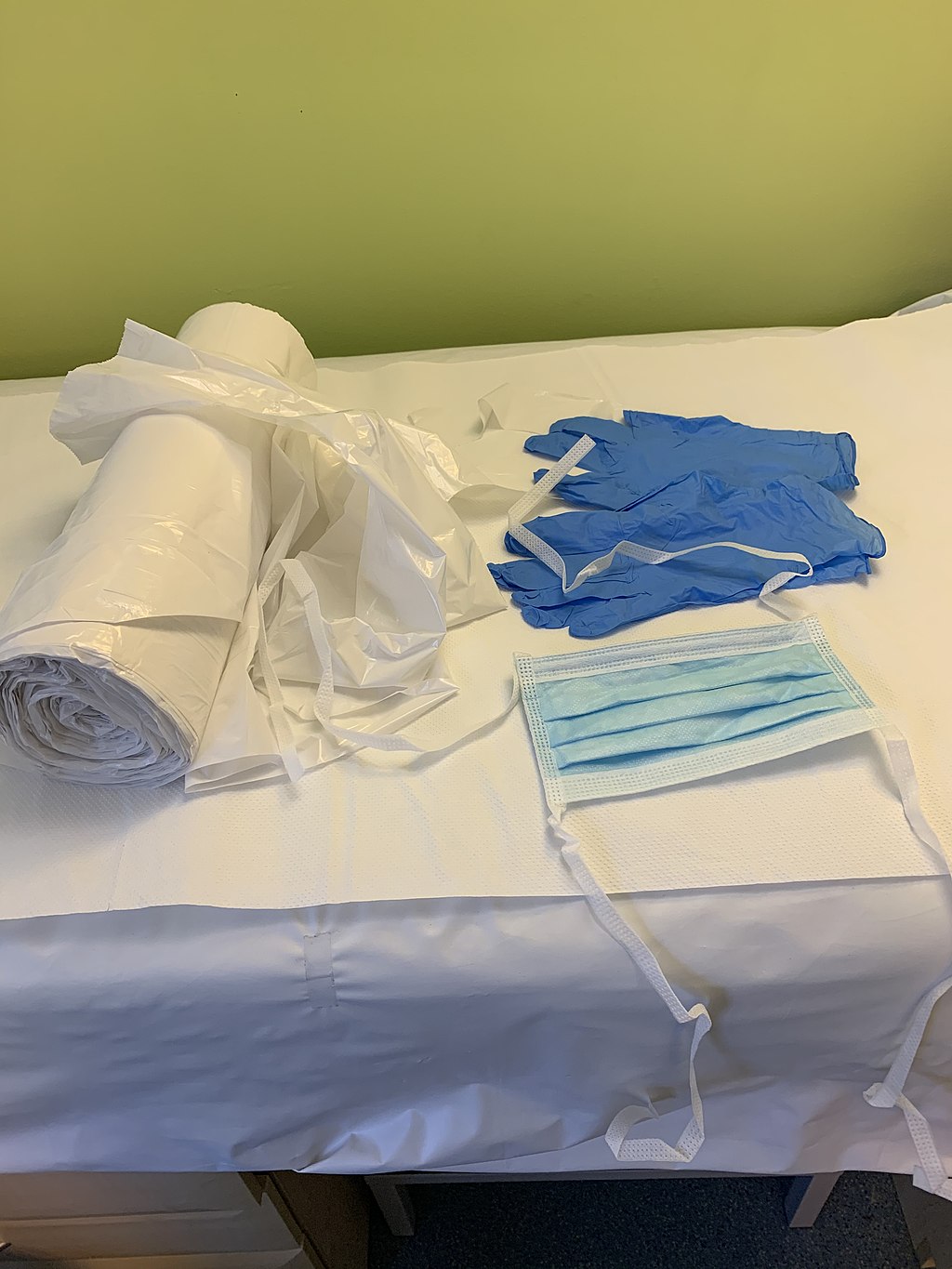 Personal protective equipment (PPE) in a British hospital, including an apron, gloves & mask. PPE is in short supply worldwide. Photo: Whispyhistory/Wikimedia Commons
Personal protective equipment (PPE) in a British hospital, including an apron, gloves & mask. PPE is in short supply worldwide. Photo: Whispyhistory/Wikimedia Commons
Facts About COVID-19 for UMHS Students
Many students have not been able to start or continue clinical rotations but some are volunteering at hospitals, and students who have matched and will start residencies this summer after graduating will be entering the nation’s healthcare settings. What should people know as they prepare to work in hospitals and health care settings during the COVID-19 pandemic?
“Students working in hospitals and healthcare settings should consider themselves on the front lines and should take all the proper precautions outlined by these facilities as well as WHO and CDC to protect themselves from exposure,” Dr. Cumby said. “Hospitals have safety protocols in place for these sorts of situations which should be strictly followed. Learn all the correct safety procedures before you set foot on the patient wards. Ensure you are always wearing the correct protective gear for whatever the procedure being performed.
“Get the proper health and safety training from the hospital so you understand how and when to use which pieces of gear. Remember that SARS CoV-2 is a respiratory virus transmitted primarily via inhalation of respiratory droplets of an infected patient. Proper precautions should be taken when working in a setting or performing a procedure that puts you at increased risk of exposure to aerosols.”
We do not know everything about the virus just yet, but there are things to keep in mind.
“SARS CoV-2 is able to survive on surfaces for at least 24 hours, so be very careful about touching things in the hospital and touching your face,” Dr. Cumby said. “You cannot help anybody if you make yourself sick, and that is true for SARS-CoV-2, or any other pathogen in the hospital. Proper preparation and protection are what lets you keep being on the front line and a benefit to your patients”
Many offices, including administrative offices of UMHS in New York City and others, are allowing employees to work remotely at home. However, there might be situations in which someone may have to come into an office for numerous reasons. What do people need to know?
“There are several important ways to protect employees from exposure in the workplace,” Dr. Cumby said. “First, ensure employees are educated about coronavirus and how to best protect themselves so that they can adopt good practices at work for mitigating spread.”
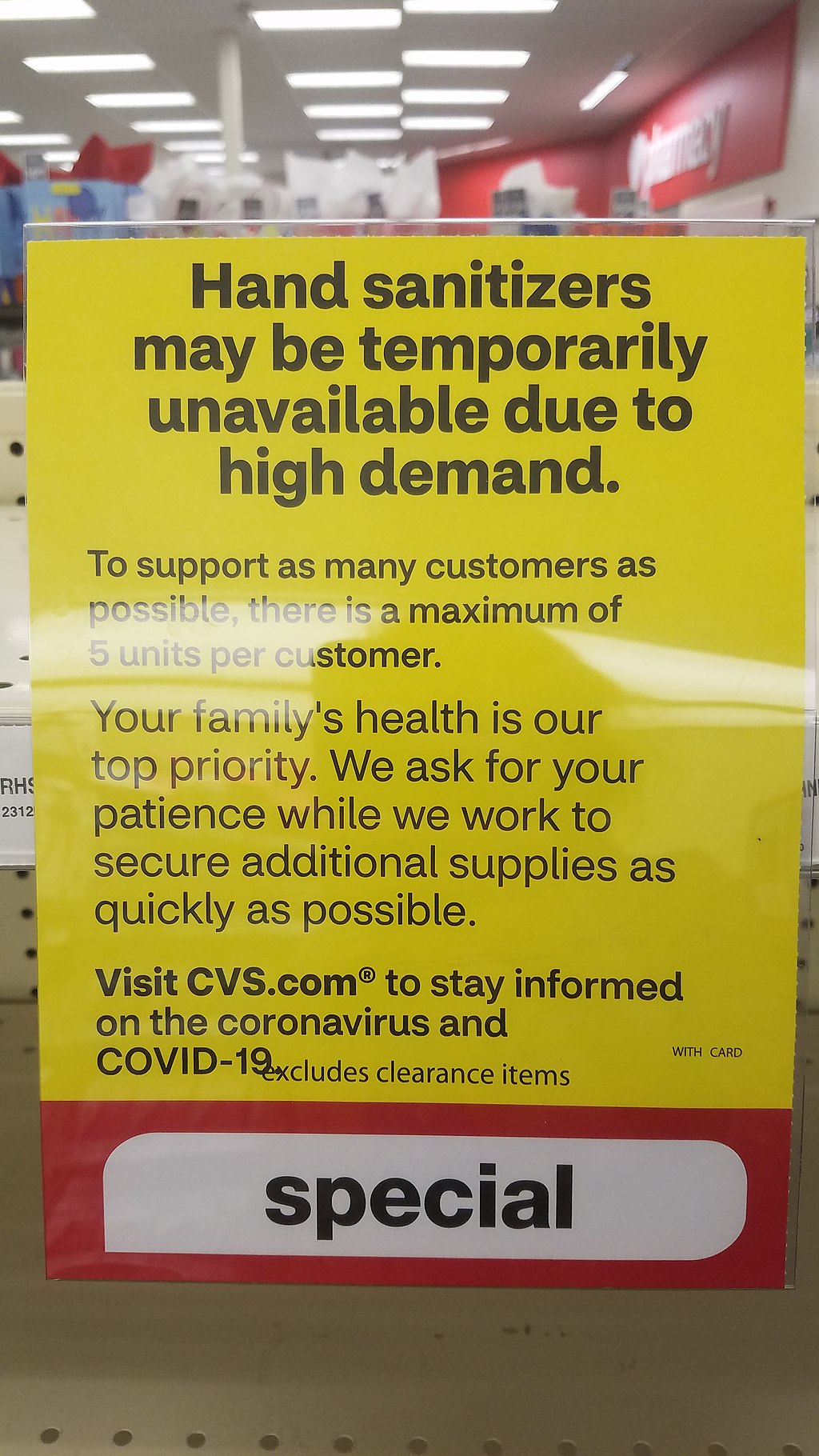
A notice in a CVS Pharmacy in the U.S. about hand sanitizers being out of stock. Photo: Breawycker/Wikimedia Commons
Dr. Cumby said office workers need to consider the following:
- “Handwashing and coughing and sneezing into the crook of your arm are practices that should be encouraged and modeled by people in senior positions.”
- “Putting signs up to remind people to wash their hands is also a good idea. Also give employees access to hand sanitizer dispensers in places for times when it is not easy to access a sink.”
- “Finally ensure office spaces and other public company areas are being cleaned daily by cleaning agents able to kill SARS CoV-2. Ensure that people who are sick stay home from work.”
- “All companies need to put the infrastructure in place so that those who are ill are encouraged to stay home, otherwise people come to work sick and risk exposing coworkers.”
- “Wherever possible, allow people to work remotely and avoid unnecessary large meetings, as these gatherings can help the virus spread. For some jobs this might not be possible, but wherever it is, it should be encouraged.”
- “For people who need to take public transit, avoid rush hour times where people are packed to capacity. When riding the subway in New York City, try to put as much distance between yourself and other passengers as possible. If someone is displaying signs of illness, try not to sit or stand near this person. Before and after riding, I would wash or sanitize my hands as during a subway ride you touch a lot of surfaces that others will also touch. Finally, be mindful of touching your face as your eyes, nose and mouth are all potential entry points for a virus like SARS CoV-2.”
Facts About COVID-19 Transmission
Washing your hands with water and soap is the best way to keep yourself from getting sick. Hand sanitizers are the next best things when traditional handwashing is not possible. Dr. Cumby said the water doesn’t need to be hot because the temperature does not kill the virus since “it is really the soap that destroys the lipid coating.”
“SARS CoV-2 is a coronavirus which means that is an enveloped virus,” she said. “Enveloped viruses have an outer envelope made of lipid (aka fat) which is sensitive to various chemicals, including ethanol and detergents. This is also why soap works great on the virus too. Most hand sanitizers consist of around 70% alcohol which does make them effective at neutralizing coronaviruses like SARS CoV-2. The key ingredient in these sanitizers is the alcohol which just needs to be above 60%”
Purell and other hand sanitizers are in short supply everywhere. What about the many “do it yourself” versions some are making with aloe vera gel and rubbing alcohol, for example?
“In a shortage, you can definitely make your own sterilization solutions for SARS CoV-2 as long as the alcohol content is 60%,” Dr. Cumby said. “However, remember that these solutions work only externally and are not effective at destroying the virus inside a person’s body.”
Many people are wearing surgical masks to go out grocery shopping, but Dr. Cumby said it is unnecessary for the general public if someone is not sick.
“I don’t believe that people who are not sick should be wearing masks,” she said. “In a situation like this where the virus is widespread and resources are limited, masks should be reserved for people that need them most. This means doctors and those who are symptomatic as recommended by the CDC. If everyone starts hoarding face masks, it means that those who need them won’t have them. For example, someone who is sick and trying to limit their chances of spreading the virus. If this person can’t get access to a mask, they might infect folks on their way to receive care, etc. This means the virus spreads. More cases mean more chances for everyone to be infected.
“Since this virus really puts a strain on our health care system, we need to give doctors and nurses access to the protective equipment they need to stay healthy working with actual cases. We really can’t afford to lose health care workers to illness at a time like this where access to health care improves survival of those severely affected.”
Will COVID-19 Cases Go Down in Summer?
Recently published studies about COVID-19 possibly waning in heat and humidity as summer approaches offer hope. What are Dr. Cumby’s thoughts?
“Most of what I have read concerning SARS CoV-2 transmission seems to indicate that the virus can travel farther between people in cooler, less humid air, which may mean the virus won’t spread as well during the summer months,” she said. “Many illnesses caused by viruses in the corona family tend to occur mostly in winter months, but this is not necessarily true for all of them. That being said, so far what we’ve seen is that SARS CoV-2 is that it is still able to spread and infect people in high humidity. There have been cases all over the world. even in places that are hot and humid, including India, Brazil, Indonesia, Thailand and Australia. So, whether SARS CoV-2 will truly be slowed by warmer weather still remains to be seen. There is truth to the observation that SARS CoV-2 is killed by heat, but we are talking temperatures above 56 Celsius (132.8 Fahrenheit) for at least 15 minutes which is well above normal atmospheric conditions, so don’t count on summer weather killing the virus.”
How does Dr. Cumby interpret the estimated range of fatality rates that we are seeing reported?
“From what I’ve read, the fatality rates can vary quite a bit between different estimates,” she said. ” The numbers have varied from place to place. For example, the initial outbreak in China reported higher fatalities while later reports were lower. It seems a major factor that explains the wide range in fatality rates we are seeing is the preparedness of health care systems to handle cases. In the beginning, fatalities were high as hospitals were not prepared for such outbreaks and didn’t have good infection control protocols in place to help mitigate coronavirus. Since the virus is spreading so easily, cases can quickly exceed many hospitals’ capacity. Generally speaking, even those vulnerable people who experience more severe infections will have lower mortality rates if they are able to access proper care.
We are already seeing hospitals in crisis mode in major cities like New York City.
“If cases grow too rapidly, the healthcare infrastructure can get overwhelmed and severe cases can fall through the cracks, inflating fatality rates,” she said. “Thus, in places where precautions are taken to slow the spread so that hospitals can treat patients, fatality estimates are lower. We are also now appreciating that more people than initially thought can be infected and experience no symptoms. These people go unreported and so fatality numbers reported would be lower if these asymptomatic people were factored into the calculations too. Overall, though, when looking at a disease that spreads easily and our global population, even small fatality rates have translated to large numbers of people on the global stage.”
COVID-19 & U.S. Health Care System & Caribbean
What implications does this disease have for healthcare systems like the US? And what about St. Kitts and other Caribbean islands?
“Diseases like COVID-19 really test the limits of healthcare infrastructure. This is equally true in the U.S. as it is in St Kitts. This disease spreads rapidly through the population because we are immunologically naïve (i.e., society has never seen this type of coronavirus before) since it spread from animals. This means that lots of people are going to catch it. Even if the fatality rate seems low as a percentage, because a lot of people will catch it, this means proportionally a lot of people will experience complications. This puts a huge burden on our healthcare system. If a lot of people catch this disease at the same time, we can end up with not enough resources for serious cases. This means that people who could be saved by supportive care can die, increasing the death toll. As a result, we are trying to ’flatten the curve’ so the healthcare system doesn’t see cases all at once but instead gets them gradually over time so it has the resources to deal with them.”
Risks for Medical Students
What risk is there to the average medical student in their 20s and early 30s?
“Fortunately, the average risk for young medical students in their 20s and early 30s is quite low overall,” Dr. Cumby said, “Most young, healthy people who contract SARS CoV-2 will experience very mild symptoms. Many may even be asymptomatic upon infection in this age range. However, that makes it easy for people in this age range to serve as vectors to transmit the virus to vulnerable segments of the population. The majority of people experiencing the more severe respiratory symptoms on average are older people typically 65 years and older or those with underlying medical conditions like type II diabetes, heart disease, etc. That’s why it’s so important everyone treat it as a serious condition. If you aren’t high risk of experience complications, you are more likely to go out, socialize and bring it to people who may not be as lucky.”
What would Dr. Cumby like to say to people under 40 who are still going about things as usual and not taking precautions?
“In order to contain the spread of this coronavirus outbreak and protect the most vulnerable members of the population, we really need everyone’s help,” she said. “Failing to take precautions gives the virus more opportunities to spread. The more it spreads, the more vulnerable people are infected and the more severe cases we will see. Too many cases can overwhelm our health system and lead to ill people not always being able to access health care. Ultimately this means more people will die. By taking precautions suggested by WHO and the CDC, you can protect your family, friends and community from the disease.”
Long-Term Effects of COVID-19
COVID-19 has already claimed more than 1,000 American lives as of March 26, 2020, with an estimated 82,000+ cases in the U.S. The virus has shut down businesses, cratered the stock market and caused mass unemployment. Is it possible to predict where we will be a year from now, in terms of global incidence and the general effects on our health care and economy?
“It is difficult to say where COVID-19 will be in a year’s time,” Dr. Cumby said. “The answer to this question will depend on a number of factors. Since this virus crossed over from animal species, we have an entire human population that is immunologically naïve (i.e., no protective antibodies) which is one reason why it is spreading like wildfire. We are currently practicing social distancing, etc. with the goal of slowing new cases. This is to limit the number of serious cases we have at a time. If too many people catch this thing together, we might not have the resources to deal with it effectively. For an example of what happens when too many catch it at once, look to countries like Italy as well as the early days in China. If we can do this, we can limit health care burdens. At the same time, people will keep getting exposed to the virus slowly and some of the population that have been exposed will hopefully experience immunity from reinfection. As this happens, fewer people will be able to spread this thing and it won’t be able to run rampant through the population anymore and you should see cases drop off. This could happen even faster if we get a good vaccine up and running. Once enough people are immune, a virus which requires people who aren’t immune to spread it will see a drastic reduction in transmission. Ideally, we want to get to this state as quickly as possible and keep the death toll low while doing it.
“My hope is certainly within a year we should have a vaccine along with people who’ve developed immunity from catching the virus which should cause cases to drop. A complicating factor in predicting the outcome is whether or not people who become infected will have lasting immunity as well as how long this immunity lasts. We don’t know for sure yet, as people are still investigating and I’ve heard people speculate both ways on the subject. Ultimately though, we should learn from this experience and be more ready for the next virus that makes a species jump. We could use better testing measures to limit spread as there are reports of people carrying this thing asymptomatically serving as reservoirs. If we could identify all those who are infected quickly and isolate them until they are no longer infected, we wouldn’t have to quarantine the world like this.”
What should the scientific and medical community do to help prevent future pandemics?
“We should probably monitor viruses in animal populations that are known to jump species better, as they are sources of potential pandemics. As we continue to expand over the world, we come into close contact with animals more commonly, contributing to this sort of spread. We should be funding research into vaccines and antiviral drugs all the time and not just when there is a pandemic to remind us that these pathogens exist. Economics is not my area of expertise, but we can all hope with the right precautions, before the disease spreads widely, we can hope to minimize the fallout.”
Advice to Ease Anxiety
Everyone is feeling anxiety with what is going on, but keeping yourself informed with facts can help ease fears.
“I strongly recommend that anyone feeling worried should seek out information from reliable sources like the CDC and WHO, and disconnect themselves from unreliable sources like social media feeds,” Dr. Cumby said. “Understanding the virus and illness better can help alleviate some of our fears that stem from the unknown as well as sensationalized accounts of pandemic. Understanding the virus, how it is spread and who is at risk also will give you information on how to best protect yourself
When Do You Need a COVID-19 Test?
COVID-19 tests are now available in most areas. When is it necessary to get tested?
” People should be tested for COVID-19 at their doctor’s suggestion,” she said. “Anyone with symptoms should call into their health care provider to seek guidance on whether or not they should be tested and follow the recommendations they receive. Doctors everywhere are working hard to keep everyone safe. Based on your presentation and history, they will be able to make a decision on whether or not you need testing. Keep in mind, this time of year, SARS CoV-2 is not the only virus in circulation, so medical personnel are carefully considering multiple factors when deciding if it makes sense to test someone.:
What else should medical students know?
“While the coronavirus pandemic is certainly scary, panic is very much the enemy in these situations,” she said. “We absolutely need to be cautious and take things seriously, but keep calm at the same time. I realize this is easier said than done but we’ve all seen firsthand the damage fear can bring about. People hoard supplies. Everyone wants to be tested for the virus. What all this does is it takes resources away from our health care system. Resources they need to fight this thing as well as reign in its spread. Much of the problem comes from all the misinformation that is out there. The rumors spreading on social media range from misleading to out and out harmful suggestions. I’d really like people to know that getting information from the wrong sources can be dangerous and contribute to the atmosphere of panic. The best places to go for the most up-to-date information on the current pandemic are sites like the CDC, WHO and the NIH. All these sites feature great information about what we currently know as well as what is currently being done in the fight against coronavirus. Reading sites like this will give you correct information and the best ways to protect yourself and your families. I would advise everyone to check them out.”
Online Resources
Centers for Disease Control and Prevention (CDC), https://wwwnc.cdc.gov/eid/article/26/6/20-0233_article
World Health Organization (WHO). https://www.who.int/
National Institutes of Health (NIH), https://www.nih.gov/
More direct links:
https://www.cdc.gov/coronavirus/2019-ncov/index.html
https://www.who.int/health-topics/coronavirus#tab=tab_1
https://www.nih.gov/health-information/coronavirus
The UMHS Endeavour and UMHS website will be updated in the coming days as news of the pandemic unfolds.
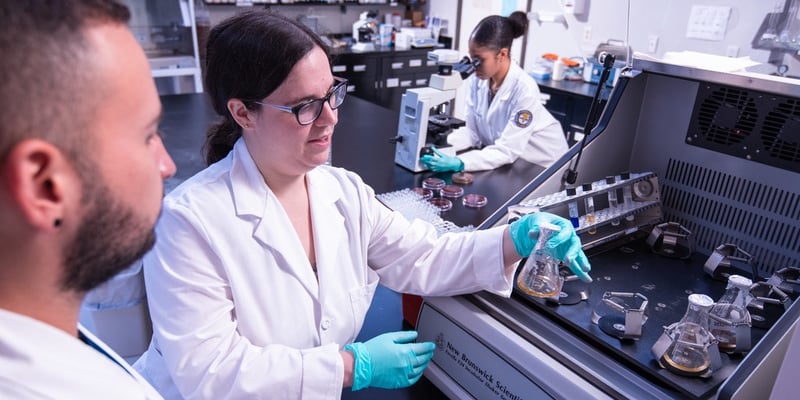
(Top photo) UMHS professor & microbiologist Dr. Nichole Cumby (center) is one of the campus experts on viruses, including COVID-19. Photo: UMHS
About UMHS:
Built in the tradition of the best U.S. universities, the University of Medicine and Health Sciences focuses on individual student attention, maintaining small class sizes and recruiting high-quality faculty. We call this unique approach, “personalized medical education,” and it’s what has led to our unprecedented 96% student retention rate, and outstanding residency placements across the USA and Canada. UMHS is challenging everything you thought you knew about Caribbean medical schools.

Scott is Director of Digital Content & Alumni Communications Liaison at UMHS and editor of the UMHS Endeavour blog. When he's not writing about UMHS students, faculty, events, public health, alumni and UMHS research, he writes and edits Broadway theater reviews for a website he publishes in New York City, StageZine.com.