COVID-19 is still a huge threat to the world, but new vaccines offer hope to eventually get the pandemic under control. With a new administration in Washington, a new Coronavirus Task Force—and President Joe Biden’s pledge to distribute 100 million doses of the vaccine within the first 100 days of his presidency—there is much promise of eradicating the virus at some point but the USA still needs to vaccinate millions of Americans. In addition, there are many myths being spread online about the vaccine, resulting in what health officials call vaccine hesitancy.
The vaccine is gradually becoming more available in the United States. The White House announced that millions of vaccines were shipped directly to US pharmacies as of February 12, 2021. Mass vaccination sites are opening in many US cities in the next few weeks. In late February, the FDA gave emergency approval to the Johnson & Johnson vaccine, requiring only one dose. The "one and done" Johnson & Johnson COVID-19 vaccine has been a proverbial game changer, allowing more and more Americans to get vaccinated. The Biden administration announced a deal on March 3rd between Johnson & Johnson and Merck to mass produce the one-shot vaccine under the Defense Production Act.
Approximately one million doses were available in 6,500 retail locations and could grow to as many as 40,000 stores, President Biden’s COVID-19 coordinator Jeff Zients said last month. The public should check local and state government "Vaccine Finder" websites to schedule appointments at local pharmacies and vaccination sites.
As new, more infectious COVID-19 strains from the UK and South Africa are discovered in the United States, getting the vaccine distributed throughout the population is more crucial than ever, and learning the facts about the vaccine is essential. The UMHS Endeavour spoke to two UMHS faculty members with expert knowledge about viruses and COVID-19 and the two FDA-approved U.S. vaccines as well as a recently vaccinated UMHS student. We discuss the facts and fallacies about the vaccine, the new RNA vaccines, the viral vector vaccine, their differences, and more. New updates on the Johnson and Johnson vaccine for the first week of March 2021 are also included, with comments from UMHS faculty. A comprehensive video about all the vaccines from Dr. Rania Siam is included at the end of this post.
Dr. Nichole Cumby & Dr. Rania Siam on COVID-19 facts & fallacies
Nichole Cumby, PhD., UMHS Assistant Professor of Microbiology, has extensive knowledge about viruses and how coronaviruses work. Dr. Cumby spoke in detail regarding the facts and fallacies about COVID-19.
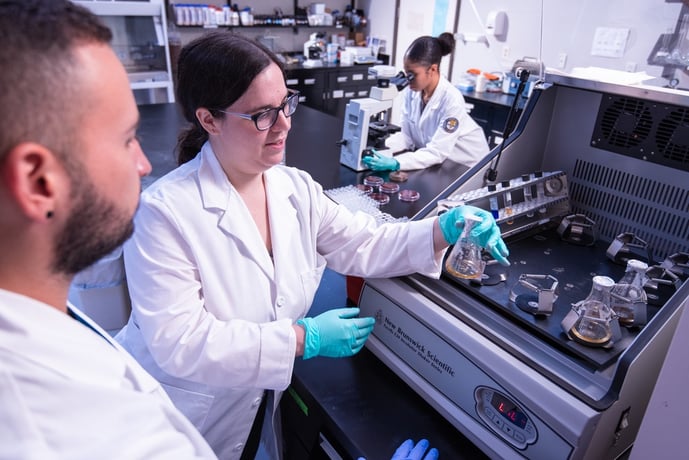 UMHS professor Dr. Nichole Cumby (center) is an expert on coronaviruses. Photo: UMHS files.
UMHS professor Dr. Nichole Cumby (center) is an expert on coronaviruses. Photo: UMHS files.
It is important to understand the elements of vaccines and how they help people build an immune response. Dr. Cumby explained the fundamentals of vaccines in an interview with the UMHS Endeavour.
“The basic idea behind vaccination is to give your body a chance to build its own response to an infection prior to the infection occurring,” Dr. Cumby said. “Normally, when a person gets exposed to a pathogen like SARS CoV-2 [the COVID-19 virus] for the first time, the body will mount an immune response to fight back. First, there is an initial response, known as the innate response. This response is non-specific and unable to clear the virus. Instead, the innate response alters general pathways in your body that the virus normally uses to replicate, slowing it down. This gives the body time to mount the second slower targeted response, known as the adaptive response, which will be able to eradicate the virus. The adaptive response is where the body raises special cells and antibodies that will target SARS CoV-2 specifically and destroy it.
“Once a person has mounted an adaptive immune response for a particular pathogen, a few memory cells for the response typically remain present and so if the same pathogen comes in again, the adaptive immune response can be turned on quickly, irradiating the pathogen before it has a chance to cause damage and make a person sick. Vaccines allow us to develop this adaptive immunity without having to actually contract the illness. Instead of getting infected by SARS CoV-2, which can make the person very sick, the goal is to expose the person to something similar enough to SARS CoV-2 that the body can make a SARS CoV-2 adaptive immune response. This way, their bodies have the adaptive response ready to fight off the virus if it infects them in the future. Most classic vaccines often use either a killed or a weakened strain of the virus in question, letting the person make a response without getting sick.”
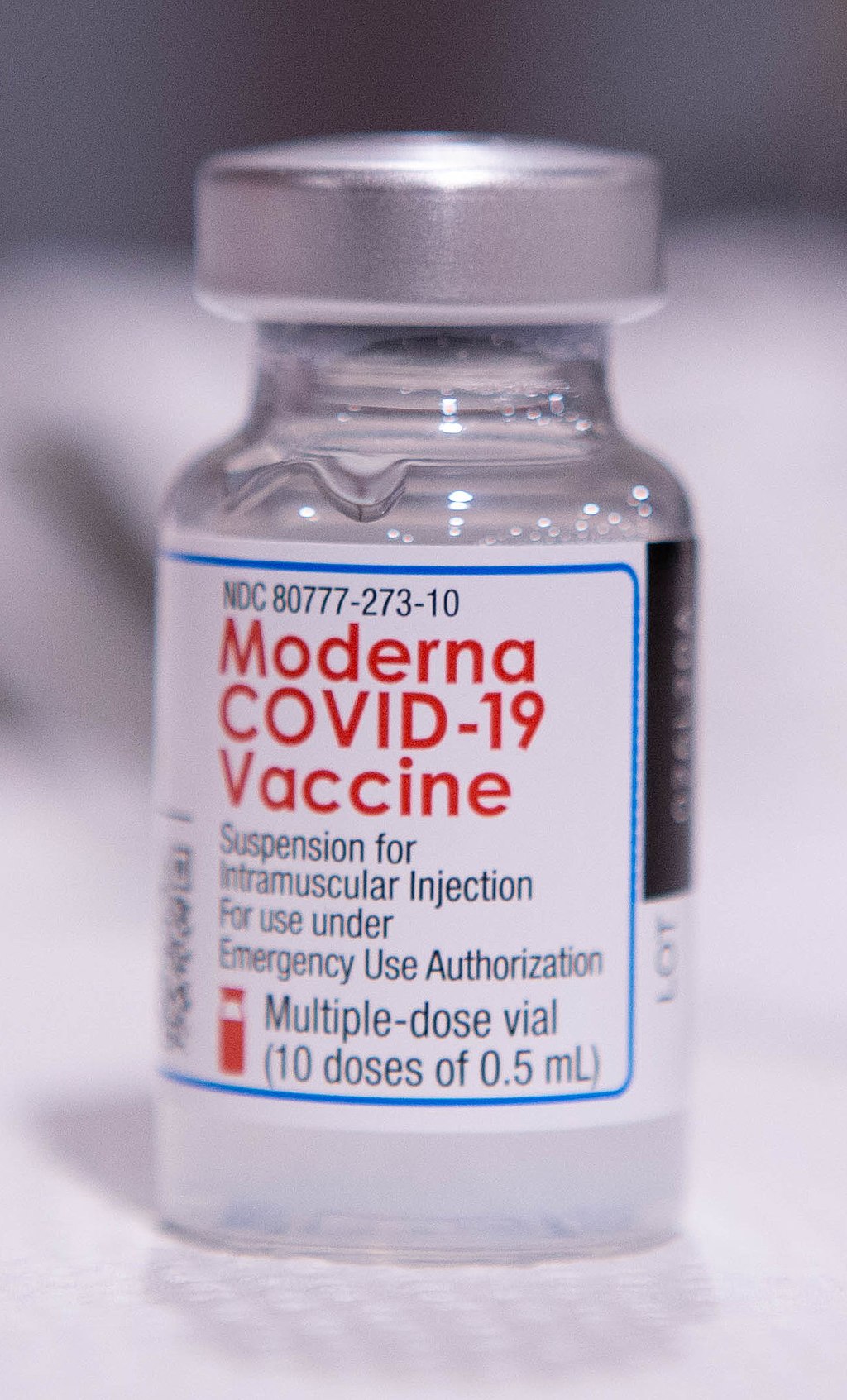 Moderna offers one of the new high-tech COVID-19 RNA vaccines approved by the FDA for use in the USA. Photo: Baltimore County Government/Wikimedia Commons.
Moderna offers one of the new high-tech COVID-19 RNA vaccines approved by the FDA for use in the USA. Photo: Baltimore County Government/Wikimedia Commons.
What is an RNA vaccine?
The Pfizer and Moderna COVID-19 vaccines are both new high-tech vaccines.
“The COVID-19 vaccine currently approved for use in the USA is a new type of vaccine known as an RNA vaccine,” Dr. Cumby said. “It still operates under the same principles as older vaccines, but actually has some serious advantages over older methods. The way this vaccine works is that the patient is injected with a piece of RNA. Now RNA (ribonucleic acid) is found naturally throughout the human body, where it is primarily used to make the body’s protein. Proteins come in a variety of shapes and sizes and perform a variety of important functions for the body. The information on what and how much protein is needed to keep our bodies functioning is actually encoded in DNA. The body makes DNA into RNA and then RNA into protein. The sequence of the protein made depends on the sequence of the DNA and RNA used. This process is not unique to humans either. Viruses are also made of proteins and they make their proteins via RNA. So, if we take a piece of RNA that codes for a viral protein, human cells can take it and make viral protein. A single viral protein on its own is not infectious; you need a complete virus to give rise to an infection. However, a single foreign protein is all that is needed to start triggering your immune system to build an adaptive response. RNA vaccines take advantage of these facts. A piece of RNA from the virus is injected, but it is only a piece; therefore, it will not cause illness but the body will still mount an immune response. The result is that without exposure to the entire virus, the body has made an immune response against a piece of SARS CoV-2. Therefore, if the virus later infects that person, the adaptive immune response to the piece of the virus is present, letting the immune system recognize and destroy the entire virus."
The vaccines are also known as "mRNA vaccines."
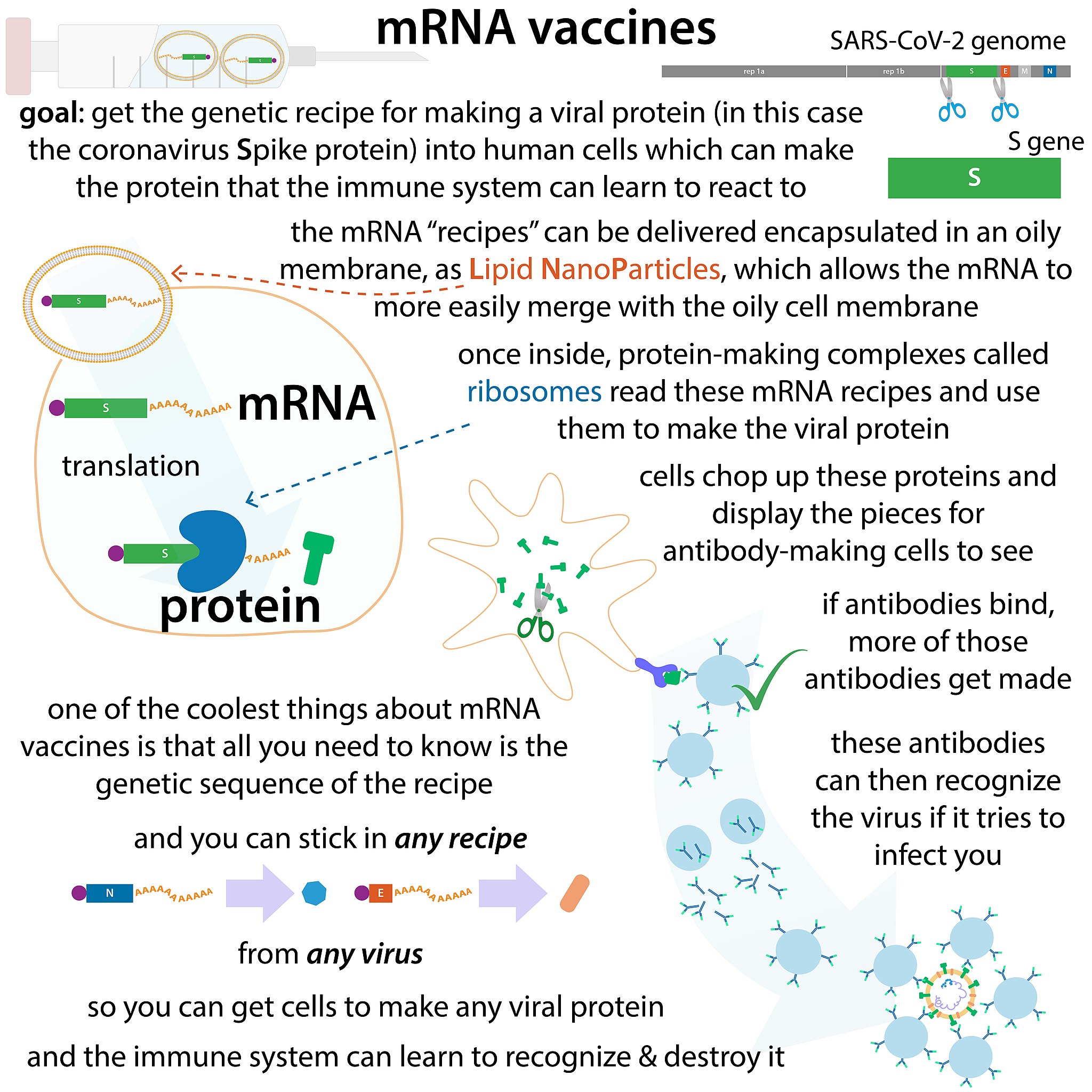 Infographic courtesy of Biochemlife/Wikimedia Commons
Infographic courtesy of Biochemlife/Wikimedia Commons
Wearing a mask before & after vaccination
Dr. Cumby spoke about the importance of getting the second COVID-19 vaccination and continuing to wear a mask and social distance before and after getting the shot to protect others.
“Unfortunately, due to the newness of SARS CoV-2, we still do not know a lot about how long immunity following infection or vaccination will last,” she said.” So even after getting the shots, it does not hurt to continue to exercise caution while scientists find the answer to this duration question. There is also a real possibility that, while getting the vaccine will protect the person from getting seriously ill with Covid-19, that same person may still be able to catch and spread the virus asymptomatically to others who have not been vaccinated yet, potentially making others very ill. Now this might be a confusing statement for some people, as they have been told the vaccine is effective. The vaccine is effective at preventing people from contracting severe disease absolutely, but it has not been tested to see if it is able to prevent person-to-person transmission. For all these reasons, masks and social distancing will still be important even after getting the shots, to protect those not yet vaccinated.”
 Dr. Rania Siam of UMHS. Photo: UMHS files.
Dr. Rania Siam of UMHS. Photo: UMHS files.
Rania Siam, MD, PhD, UMHS Course Director and Professor of Microbiology, also explained the need to wear masks and social distance after being vaccinated.
“I believe that the rationale for wearing masks and social distancing after receiving the COVID-19 vaccine is because 1.) studies showed that the vaccine protects from symptoms of COVID-19 and not from contracting the vaccine and becoming an asymptomatic carrier; and 2.) until a large number of the population is vaccinated (60 to 80%), we haven't stopped the pandemic,” Dr. Siam said.
One of the biggest misconceptions about the vaccine is that it won’t work because some feel clinical trials and approvals were rushed. Is this really cause for concern?
“Actually, I think companies so far have been doing an admirable job of not caving in to public pressure and bypassing safety protocols,” Dr. Cumby said. “The outcry for vaccines has been very vocal as people see this as a way to return to normal. Despite the public’s intense pressure for a vaccine since this all started, companies have been following the normal protocol for new vaccine approvals which includes all relevant safety checks. They have been doing everything to proceed quickly while still following all the relevant safety protocols. Additionally, no vaccine becomes available in the US without approval by the FDA. The two SARS CoV-2 vaccines now available in the US are, therefore, both FDA approved. This is not an easy hurdle for new vaccines and drugs to clear as the point of the FDA is to protect consumers against bad drugs. There are drugs that seem to show early promise that do not secure FDA approval for safety reasons.”
 The newly approved Johnson & Johnson vaccine only requires one shot. Photo: Courtesy of Johnson & Johnson.
The newly approved Johnson & Johnson vaccine only requires one shot. Photo: Courtesy of Johnson & Johnson.
1 dose of Johnson & Johnson is helping combat pandemic
The new Johnson & Johnson vaccine recently received emergency approval from the FDA and it only requires one dose. We spoke to UMHS professors Dr. Siam and Dr. Cumby about the new vaccine.
"On Feb 27, 2021, the US FDA approved the emergency use of the Johnson & Johnson COVID-19 vaccine," Dr. Siam said. "This is the single one-dose COVID-19 vaccine. The company's website indicates that it’s 85% effective in preventing severe infection."
Because Americans cannot choose which brand or type of COVID-19 vaccine they want, it is important to get the vaccine that is offered when it is your turn to get a shot.
"At this point, I would recommend that individuals get a COVID-19 vaccine, irrespective of the type of the vaccine, [because it] will protect individuals from developing severe infections with the coronavirus COVID-19," Dr. Siam said. "If enough people are vaccinated, this allows us to establish a 'population immunity'— also known as 'herd immunity'— note that this would require the vaccination of a substantial population. This is the only way I can think of to end the pandemic and for life to resume back to normal (if applicable)."

Dr. Cumby of UMHS echoes these sentiments and noted that the Johnson & Johnson is slightly different but will ultimately protect people from getting sick from Covid.
"The new Johnson & Johnson vaccine is a viral vector vaccine. It works very similarly to mRNA vaccines from Pfizer and Moderna. The end result of using either of these vaccines is that our human cells make a piece of viral protein which then our immune system is able to mount a response. The things that make the Johnson and Johnson vaccine exciting is that a single dose confers strong protection. This is very useful when you are dealing with a situation like the one we are in where you have to vaccinate a large number of people."
Dr. Cumby notes that people should understand that clinical trials on all three vaccines were done separately and comparing the efficacy of each oversimplifies things.
"When it comes to deciding which vaccine looks best, many people have been directly comparing these efficacy numbers," she said. "Unfortunately, it is not as simple as that. The studies are not directly comparable. The biggest reason for this is that Moderna and Pfizer studies were not done at the same time as the Johnson and Johnson study. The Johnson & Johnson studies were conducted later when new variants of coronavirus had already emerged. The advent of new strains could easily alter efficiency. This is why it is not a simple matter of seeing which numbers are highest to decide what vaccine is best. Ultimately, all vaccines on the market right now are showing excellent protection against severe COVID-19 hospitalization and death. So, all of them are valid and protective. Therefore, I would not make my decision on which vaccine to take based on efficacy but rather based on availability. Here in St. Kitts, for example, the AstraZeneca vaccine has been delivered and made available and so this is the vaccine that I am using.”
Why COVID-19 vaccine will not make you sick
Contrary to many myths, getting the COVID-19 vaccine will not make you sick.
“I think the confusion on this subject is the result of a general lack of understanding of vaccines and how they work and the different varieties that exist,” Dr. Cumby said. “There are some vaccines out there that do use weakened viruses known as attenuated vaccines. These vaccines generally do not make a healthy person ill but can make someone with a weakened immune system ill. However, both the Moderna and Pfizer SARS CoV-2 vaccines are a new type of vaccine known as an RNA vaccine. Unlike the attenuated vaccines, there is no actual virus in this vaccine. Instead, this vaccine consists of a piece of RNA. This RNA is not infectious as it only codes for a piece of the virus, not the entire virus. Since the RNA will only be made by the body into a small piece of SARS CoV-2 and not the entire virus, it cannot give a person Covid-19. In order to get Covid-19, the entire virus is required. Now some people who get the vaccine will experience minor cold and flu symptoms. This response is not due to actual virus but actually it is due to your immune system mounting that protective response.”
Since the COVID-19 vaccine is an RNA vaccine, as previously stated, there are no live viral agents in it. This means it is safe for people with compromised immune systems as well as pregnant women.
Dr. Siam further explains why a COVID-19 vaccine does not make you sick.
“Generally speaking, some vaccines can result in mild illnesses (similar symptoms to the infection the vaccine protects from) but they are usually much milder than the illness itself.”
Vaccines & new COVID-19 mutations
Much has been reported in the media about new COVID-19 mutations. Will the current vaccines protect people from these?
“With respect to the new variants (UK and South African strains) and the Moderna and Pfizer vaccines, so far preliminary data shows that the older vaccines do still seem to be at least somewhat protective against these variants,” Dr. Cumby said. “However, there is some early data that shows that certain mutations do result in antibodies generated by the current vaccines being less potent (meaning they do not bind to the mutant strains as well). At this time, though, it remains to be seen how this drop in potency will translate in people’s bodies. The antibodies generated from the vaccines, though less potent against the newer strains, might still be able to recognize and bind the new viral variants enough to prevent severe illness, especially if they are being produced at high concentrations. However, many companies are erring on the side of caution and developing boosters formatted for the new variants.”
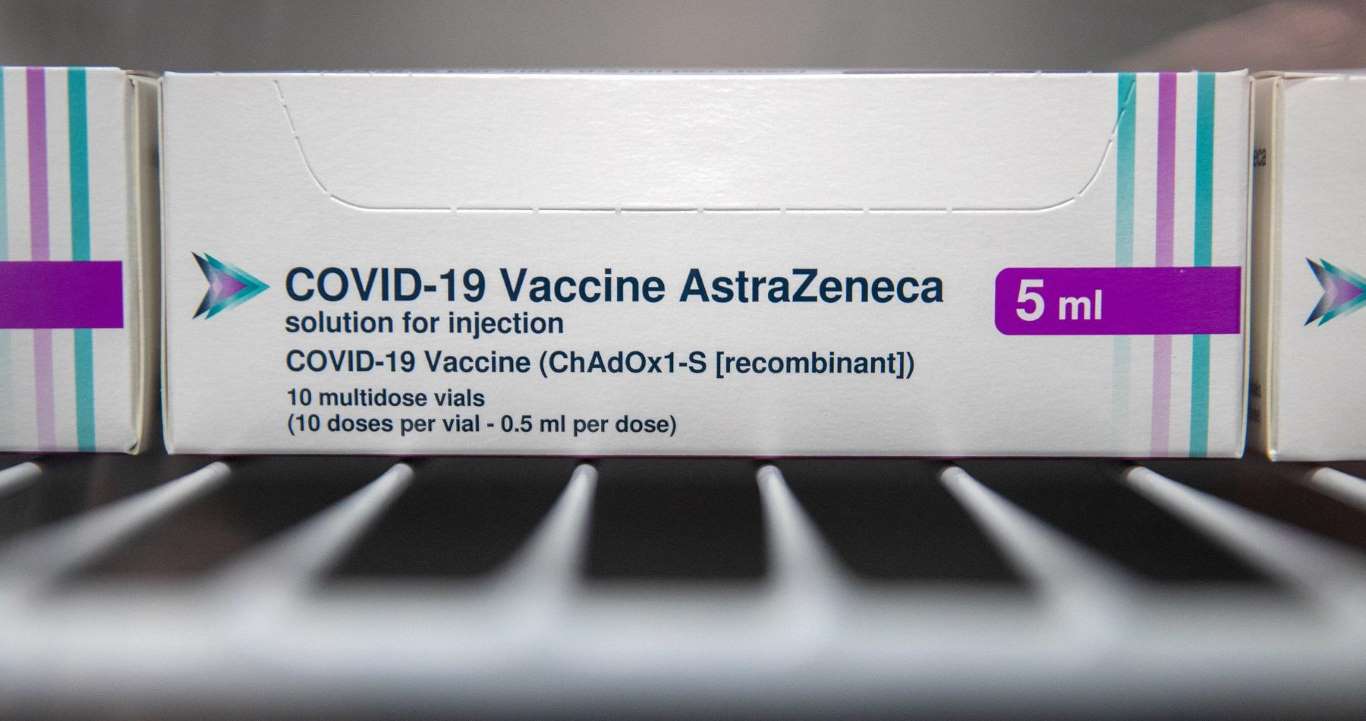 A box of AstraZeneca COVID-19 vaccine in a refrigerator at a stadium in Bristol, United Kingdom. The AstraZeneca version is a viral vector vaccine not yet approved by the FDA in the USA. Photo: Andrew Matthews / POOL / AFP Astrazeneca-Oxford/Wikimedia Commons.
A box of AstraZeneca COVID-19 vaccine in a refrigerator at a stadium in Bristol, United Kingdom. The AstraZeneca version is a viral vector vaccine not yet approved by the FDA in the USA. Photo: Andrew Matthews / POOL / AFP Astrazeneca-Oxford/Wikimedia Commons.
Viral vector vaccines: How are they different?
Although not yet approved by the FDA in the United States, the Johnson and Johnson and AstraZeneca vaccines have received a lot of media coverage. Dr. Cumby explained how these injections—known as viral vector vaccines—work and how they differ from the Pfizer and Moderna shots.
“With respect to the Johnson and Johnson and AstraZeneca vaccines, these are some new options coming rapidly up the pipeline,” Dr. Cumby said. “These vaccines are using a different platform to get around the main weakness of RNA vaccines: stability. RNA degrades easily and needs to be stored at very cold temperatures around -70 C. This presents challenges for distribution. AstraZeneca and Johnson and Johnson’s vaccines are aiming to overcome this limitation by using a different type of vaccine: the viral vector vaccine. These vaccines take another virus known as adenovirus and modify it so that it cannot replicate in humans. They use these modified viruses to transport a piece of the SARS CoV-2 genome that codes for a viral surface protein. Like with the RNA vaccine, since this is only a piece of SARS CoV-2, it is not capable of making the full SARS CoV-2 virus and thus causing COVID-19. However, that piece is enough for our human cells to make some viral surface protein which then the immune system can mount a response against, protecting against a future SARS CoV-2 infection. The strategies for both RNA and viral vector vaccines are ultimately the same: getting our own cells to produce a small piece of SARS CoV-2 without us having to be infected by the entire virus so we can develop an immune response. The main advantage of this system compared to the RNA vaccines is stability. Early data also is showing even with just a single dose, these viral vector vaccines can be effective in preventing severe illness. Additionally, the AstraZeneca and Johnson and Johnson vaccines are significantly cheaper than RNA vaccines.”
Are vector vaccines better than RNA vaccines?
“That is a difficult question to answer at this time since different companies may be using different measures of vaccine efficacy,” she said. “For example, one company may be measuring vaccine efficacy using severe hospitalizations as a measure. Another might be looking at antibodies or doing RT PCR to see if participants are infected. If the endpoints are not identical, one cannot easily cross compare vaccines to see which is the best. So far data indicates that all vaccines are protective against severe illness though.”
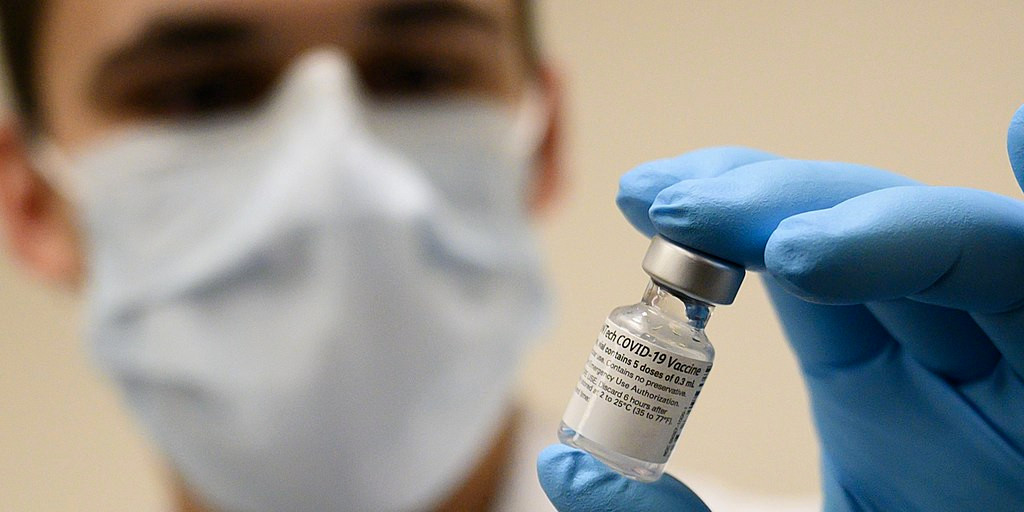
A healthcare worker with the Pfizer COVID-19 vaccine. Photo: Wikimedia Commons.
Do you need to get vaccinated if you’ve had COVID-19?
Is it necessary to get the COVID-19 vaccine if you’ve already had Covid? News reports have noted that people who got sick from the virus may only have antibodies for a few months. So, if one has already become ill from the virus, does one still need the vaccine?
“I would definitely recommend getting the COVID-19 vaccine even if you have already had Covid,” Dr. Cumby said. “The reason for this recommendation is because at the present moment, we are unsure how long the immunity lasts following the infection. There is some evidence from studies on other coronaviruses that immunity following infection with the entire virus may be short-lived. However, since these studies are on the seasonal cold variants, which are distinct from the pandemic strain, these results might not be applicable to COVID-19. So far, there has not been as much work done concerning long-term immunity for SARS CoV-2 since it has not been around long.”
Dr. Cumby said too little is known about previously infected individuals and immunity.
“The reality is because this virus is new and different viruses behave differently when it comes to lasting immunity, we just do not know for sure yet. Most data I have seen so far does support the idea that antibody levels drop following infection. However, at the moment, we are not sure if declining antibodies means that a person is vulnerable to reinfection. Historically, antibodies are often used as a marker of immunity status to a particular pathogen. For certain pathogens, this works well, but there is evidence to suggest that may not be true for all pathogens. During a viral infection, antibodies are not the only response to a virus. One of the main immune responses against viral infections are special cells called T-cells which seek out and destroy infected cells. This means that antibodies may decline but other immune components may still be present and protective. So, whether the declining antibodies really means declining immunity in this case is still being assessed. However, what is clear from this finding is that using antibodies to test for previous SARS CoV-2 exposure that occurred longer than 90 days is not feasible.”
Dr. Siam also believes people who have already been sick from the virus need to be vaccinated.
“So far the answer to this question is yes—since we don't have sufficient information on the immunity duration following infection with COVID-19,” Dr. Siam said. “Note that cases with reinfection with COVID-19 have been reported.”
Combating anti-vaccine myths
There is a lot of anti-vaccine information on social media and in some local TV news reporting around the country. One of the most absurd myths circulating online is the Covid vaccine contains microchips to track people. Dr. Cumby stresses the need to check sources and be skeptical when one reads outrageous claims about what vaccines can and cannot do.
“One of the great things about America as a country is the right to free speech,” she said. “This is also an important part of scientific discourse, too. In science, one never turns a blind eye to alternate ideas when seeking the truth. In order to find the truth, everything needs to be thoroughly investigated. However, when all these ideas are put on the table, how does one decide which ones are plausible and which are not? A true scientist will test them all. They will not decide just to test one thing because they think this is the answer. At the end of this process, the ideas that stand up to scrutiny become accepted truths. For subjects I am not directly working on myself and not actively experimenting on in this fashion, I look to people doing that same rigorous testing process on those subjects. I never blindly believe anything and I consider my sources carefully. Does it make sense that this person would have knowledge and experience in this area? Do their experimental methods and data hold up to scrutiny? If they are not an expert, are the sources they used reliable? This is not just true for scientific information but also true for other areas of life. If my mechanic is giving me a hot stock market tip, do I up and buy up a grand of the stock because he says so? My mechanic might have a great tip, but I am going to fact check it before I make a large financial commitment like this.”
She urges people to be careful about believing things just because they are posted on social media, considering this is how many people get news these days.
“Now, one of the tricky things in life that makes it easy for people to be paranoid is the ability of anyone anywhere to put information out and make it seem legitimate. Think Facebook posts, websites, etc. that all seem trustworthy at a glance. However, you should always read carefully and consider the information source. If there is no citation to a well-performed peer-reviewed study, just a bunch of websites or self-published articles, I generally do not believe it. I encourage everyone to be similarly critical. Check facts. Investigate all sides of an issue thoroughly before making important decisions.”
Keep in mind that sharing false information with friends and family can have serious consequences.
“I think whenever you provide information on a subject, you have a responsibility to ensure it is as accurate as can be, for the sake of the person to whom you are speaking,” Dr. Cumby said. “Be responsible when you are reporting information and avoid the temptation to spread information you have not vetted. Always cite your sources. There is a real danger with spreading misinformation. People closest to you are the ones that tend to trust you and therefore you tend to have a greater ability to influence their decisions. This means that if the advice you are giving is wrong, the people you care about are the ones making wrong decisions based on your information. This can lead to them being hurt.”
Has Dr. Cumby been vaccinated yet?
“I plan to get the vaccine myself as soon as it is available for me. I am advising family and friends to do the same. I feel this demonstrates my opinion on this vaccine better than anything else I could say on the subject.”
Some side effects from the vaccine have been reported, Dr. Rania Siam said.
“The FDA reports indicate ‘Throughout the safety follow-up period to date, there were three reports of facial paralysis (Bell’s palsy) in the vaccine group and one in the placebo group.’ Currently available information is insufficient to determine a causal relationship with the vaccine. There were no other notable patterns or numerical imbalances between treatment groups for specific categories of adverse events (including other neurologic, neuroinflammatory, and thrombotic events) that would suggest a causal relationship to mRNA-1273."”
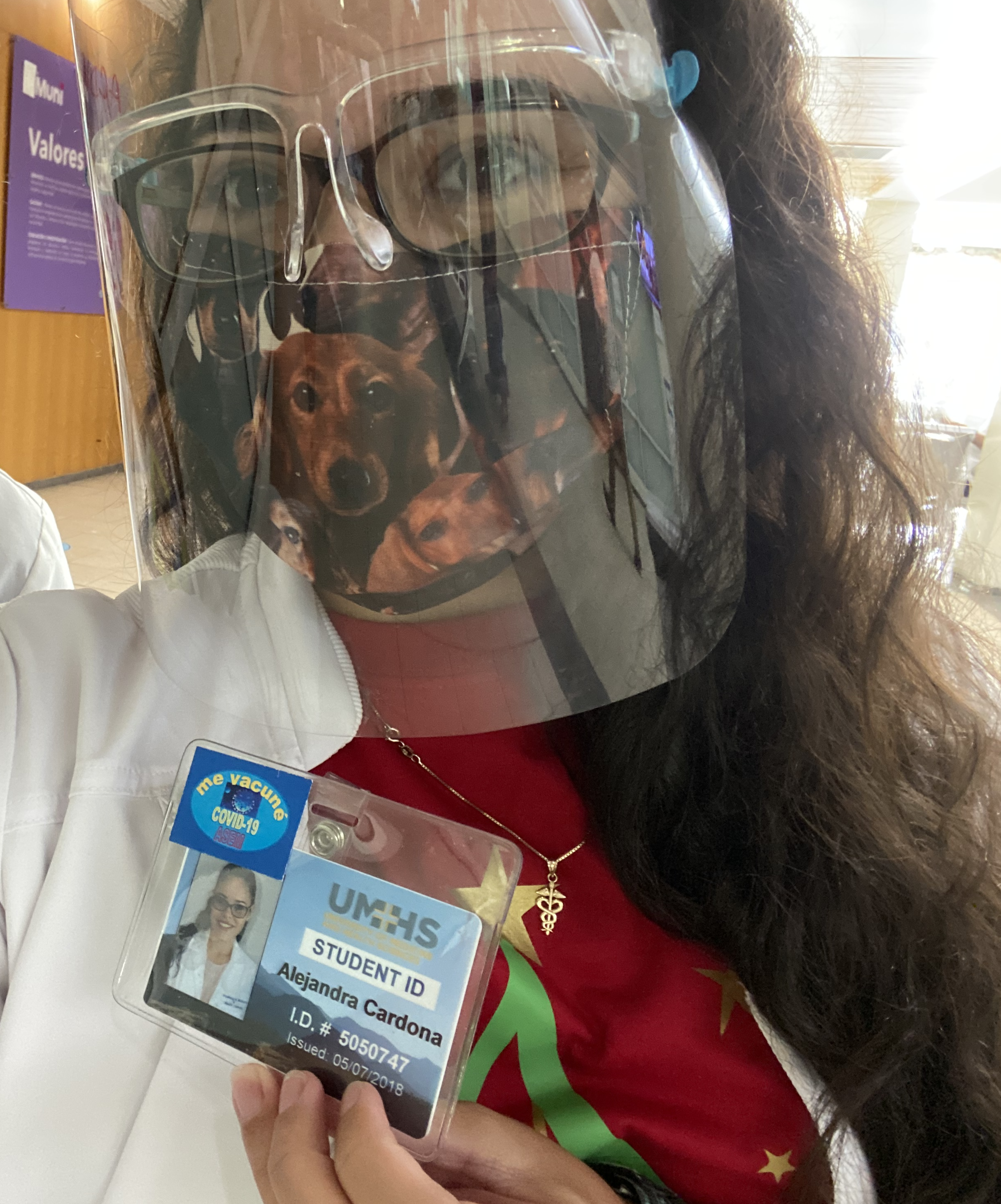 UMHS student Alejandara Cardona Del Valle right after getting her first COVID-19 vaccine at San Juan City Hospital in Puerto Rico. Photo: Courtesy of Ms. Cardona Del Valle.
UMHS student Alejandara Cardona Del Valle right after getting her first COVID-19 vaccine at San Juan City Hospital in Puerto Rico. Photo: Courtesy of Ms. Cardona Del Valle.
UMHS student discusses getting vaccine
UMHS student Alejandra Cardona Del Valle received her first vaccine in December 2020. She discussed why she felt it was necessary to get the shot. She recently completed a rotation at San Juan City Hospital in Puerto Rico.
“I got it because I feel it is our responsibility to end this pandemic as soon as we can,” she said. “I got it for my friends, family, co-workers and for me. If there is a way we can end this pandemic, getting vaccinated is definitely an important step.”
She said she experienced no side effects. “It was very similar to what I feel after the flu shot; just some mild discomfort at the area but nothing major.”
Ms. Cardona Del Valle said with the Pfizer and Moderna vaccine, it’s vital to get the second shot within 21 days after the first, if possible, and continue to wear masks and social distance.
“For maximum efficacy, it is important to get the second shot. This happens with many vaccines that need even four doses to be effective and keep building up and reinforcing that immune response. Even though some of us are getting the vaccine, it is important that we all still wear a mask and keep the six-feet rule to protect those who are not immune yet. I know the process may seem slow, but we are making progress and it is crucial to follow the recommendations of health experts to end this pandemic as soon as possible.”
She said people who think the Covid vaccines aren’t safe because they were developed quickly are wrong.
“I think it was quickly developed because it was quickly needed,” she said. “Since COVID-19 became a worldwide problem in less than a year, many scientists from different countries shared their knowledge. Also, the fact that this vaccine is an mRNA vaccine could explain the fast development. I'm no immunization microbiologist but I'm assuming that isolating a protein is easier than manipulating the whole virus.”

UMHS student Alejandra Cardona Del Valle. Photo: UMHS files.
She also stressed that the vaccines will not actually give people COVID-19.
“None of the vaccines that are being developed use the live virus, so you would not get sick from vaccination. Even the CDC talks about this misconception on their website; you should check it out.”
She said people should not listen to the many absurd vaccine myths and conspiracy theories, such as vaccines containing microchips to track the vaccinated.
“These statements sound like a ‘Black Mirror’ episode from Netflix—ha, ha,” she said. “Don't get me wrong, I love the series, but COVID-19 is actually happening and I doubt that the government would prioritize stalking people with microchips over global health and ending the pandemic.”
People need to help end the pandemic by getting the vaccine when it becomes available to them.
“I want to encourage everyone who has access to the vaccine to get it. I can't wait to hug my family and friends again. I know many of you feel the same way. But there is a way we can start the ending of this pandemic and these scientists worked hard developing these vaccines. As I mentioned earlier, the process may seem slow but we are making progress one shot at a time. Go get vaccinated and let's end this together.”
Video from Dr. Rania Siam of UMHS about COVID-19 vaccines
Sources on COVID-19 vaccines
More info on RNA vaccines: https://www.frontiersin.org/articles/10.3389/fimmu.2020.608460/full
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/mrna.html
More info on FDA approval of Covid vaccines:
Safety study for Pfizer vaccine: https://pubmed.ncbi.nlm.nih.gov/33301246/
Vaccine ingredients:
Pfizer vaccine: https://www.fda.gov/media/144414/download
Moderna vaccine: https://www.fda.gov/media/144638/download
More sources: https://www.nature.com/articles/s41591-020-1083-1
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0244126
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7641391/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7553736/
https://www.fda.gov/media/144434/download
(Top photo) Top squares: File of the new Johnson and Johnson COVID-19 vaccine; UMHS student Alejandra Cardona Del Valle; Moderna COVID-19 vaccine. Bottom squares: UMHS professor Dr. Rania Siam; Ms. Cardona Del Valle after receiving her first Covid shot; UMHS professor Dr. Nichole Cumby at work in her lab. Photos from UMHS files & Wikimedia Commons. Collage: Victoria Ross.

Scott is Director of Digital Content & Alumni Communications Liaison at UMHS and editor of the UMHS Endeavour blog. When he's not writing about UMHS students, faculty, events, public health, alumni and UMHS research, he writes and edits Broadway theater reviews for a website he publishes in New York City, StageZine.com.

















