Dr. Melissa Alvarez ’17 recently started a new position as the Chief Cardiovascular Disease Fellow at Danbury Hospital in Connecticut. Dr. Alvarez completed an Internal Medicine residency at Mercy Catholic Medical Center in Darby, PA in June 2021. Dr. Alvarez is a Cardiovascular Disease Fellow at Danbury Hospital and will be starting an Interventional Cardiology fellowship in July 2024 at Summa Health.
Dr. Alvarez works regularly with the American College of Cardiology and currently serves on the Connecticut Chapter of Women in Cardiology Section, as Chief FIT for the ACC Young Scholars Program, and was a mentor in the IM Resident Program.
Dr. Alvarez is a board-certified physician and a 2017 graduate of UMHS. In her new role as the Chief Cardiovascular Disease Fellow at Danbury Hospital, she manages all of the fellows, creates schedules, coordinates educational programs, and acts as a liaison between the fellows and program faculty. Dr. Alvarez is also the Fellow in Training Leadership Director of the Young Scholars Program at the American College of Cardiology, where she mentors high school and college students interested in cardiology. She highlights the importance of giving back to medically underserved communities and developing countries, as it not only helps those in need but also provides a deeper appreciation for the resources available in developed countries. Dr. Alvarez emphasizes the need for primary care, regular check-ups, and lifestyle changes to maintain heart health and prevent cardiovascular disease. She also discusses the exciting advancements in cardiology, such as ablation techniques for arrhythmias and non-invasive valve replacements. Dr. Alvarez expresses her gratitude for the professors at UMHS who supported and rooted for their students' success, and she looks forward to the launch of the UMHS Alumni website and the opportunity to reconnect with fellow alumni. She encourages current and prospective students to reach out to her on LinkedIn for any questions or advice.
UMHS spoke to Dr. Alvarez on a winter day when she had a rare break.
 Dr. Melissa Alvarez at the American College of Cardiology right before the ACC Young Scholars Camp Cardiac presentation in Washington, D.C. Photo: Courtesy of Dr. Alvarez.
Dr. Melissa Alvarez at the American College of Cardiology right before the ACC Young Scholars Camp Cardiac presentation in Washington, D.C. Photo: Courtesy of Dr. Alvarez.
New position as Chief Cardiovascular Disease Fellow in CT
UMHS Endeavour: Can you tell us a little bit about your new position as Chief Cardiovascular Disease Fellow at Danbury Hospital in Connecticut?
Dr. Melissa Alvarez: I'm currently in the final year of my general cardiology fellowship at Danbury Hospital in Danbury, Connecticut, a site that a lot of UMHS students may be aware of. We have a psych rotation there. As the chief fellow, my job is basically being the manager of all of the fellows. I'm in charge of making everyone's schedule. If someone calls out, I find coverage. I also help with developing the educational curriculum. I'm the liaison between the fellows and our program director and faculty, tweaking things with the fellowship and bringing up concerns we have, bringing up faculty concerns to the fellows. It's more administrative, but it's a good role to learn that side of medicine because in the future, no matter what job you get, you have to deal with administration so, learning to do that administrative piece has been interesting.
You are also a fellow in training leadership director of the Young Scholars Program at the American College of Cardiology. Can you please share some of what this involves?
Sure. The American College of Cardiology is the big national US group for all cardiologists across the country. As part of their diversity and inclusion initiative, they started the Young Scholars Program. This is a program that takes high school and college students and immerses them into the world of cardiology. So last year was the first year that I had the opportunity to volunteer with this group. We have a group of fellows that puts together programming for these students every week. We teach them nuts and bolts about cardiology, what an EKG is, and what is the anatomy of the heart because they're high school college students, so we try to get down to their level. We also had the opportunity to put together a camp for them. They were flown to the headquarters of ACC, which is in Washington DC. We had a pathologist come in and show them actual hearts in various disease states and what normal is. They got to echo each other with some echo probes on an iPad. So, it's been really fun.
This [past] year [2023], they kept me and one other fellow and we are in charge of the team of fellows this year and guiding them. It’s been really fun being able to be a part of that program. A lot of these kids are underrepresented in medicine. The fact that they get to go to D.C., some of them have never flown on a plane before. Some of them have never stayed in a hotel. So being able to be a mentor to those kids has been great. And seeing how smart they all are, I don't know if I would get into medical school now with some of the stuff these kids are doing. They've published papers. They've been presenting places. They've been volunteering. So, it's actually really inspirational to get to work with them as well. It’s been a great experience.
That sounds amazing. And Dr. Alvarez, you're going to be starting an interventional cardiology fellowship in 2024 at Summa Health. Can you tell us a little bit about what your goals are for this?
I'm going to be doing a one-year interventional cardiology fellowship. Interventional cardiology is the group of doctors that take care of coronary artery disease from a procedural perspective. So, when you hear someone has a heart attack and they get brought to a lab and they get a stent placed, the interventional cardiologist is the one that's doing that procedure. I'm someone who's always liked procedures. I like being hands-on. I don't enjoy being in the office all the time. So, I'm really excited that I get to do this role.
The other thing interventional cardiologists get trained to do is valve replacements. There are patients where surgery isn't a great option for them because they're too high risk or they've had surgery previously, so redoing surgery would be difficult. There are procedures in place to replace valves by going in through the arteries in the legs so that you don't have to cut someone's chest open. So, I'll be able to do that as well.
 Dr. Melissa Alvarez at the American College of Cardiology in New Orleans, LA. Photo: Courtesy of Dr. Alvarez.
Dr. Melissa Alvarez at the American College of Cardiology in New Orleans, LA. Photo: Courtesy of Dr. Alvarez.
Really, my goal for this year coming up is to just work as hard as possible to get as strong and as good in these procedures as I can. A year seems like a long time, but it's really not. So, it's going to be challenging and I'm just hoping I can focus and just get as technically good as I can.
It looks like you're doing some really amazing and important work. And you didn't actually start out in cardiology. You completed your internal medicine residency at Mercy Catholic Medical Center, in Pennsylvania. What were some of the highlights of your residency there?
Internal medicine is the first step to getting a cardiology fellowship or an interventional cardiology fellowship. Mercy Catholic Medical Center is actually just right outside of Philadelphia, Pennsylvania. It is a community hospital. So, I feel like the best part was how I was able to build my confidence in my own decision-making skills. When you first come out of med school and you first start residency, you don't feel like you know anything. You feel like you've been in school for four years, but the first time a nurse comes up to you with a question, you're like, no, I have no idea. And you run to your senior resident or you run to your attending and you're asking questions.
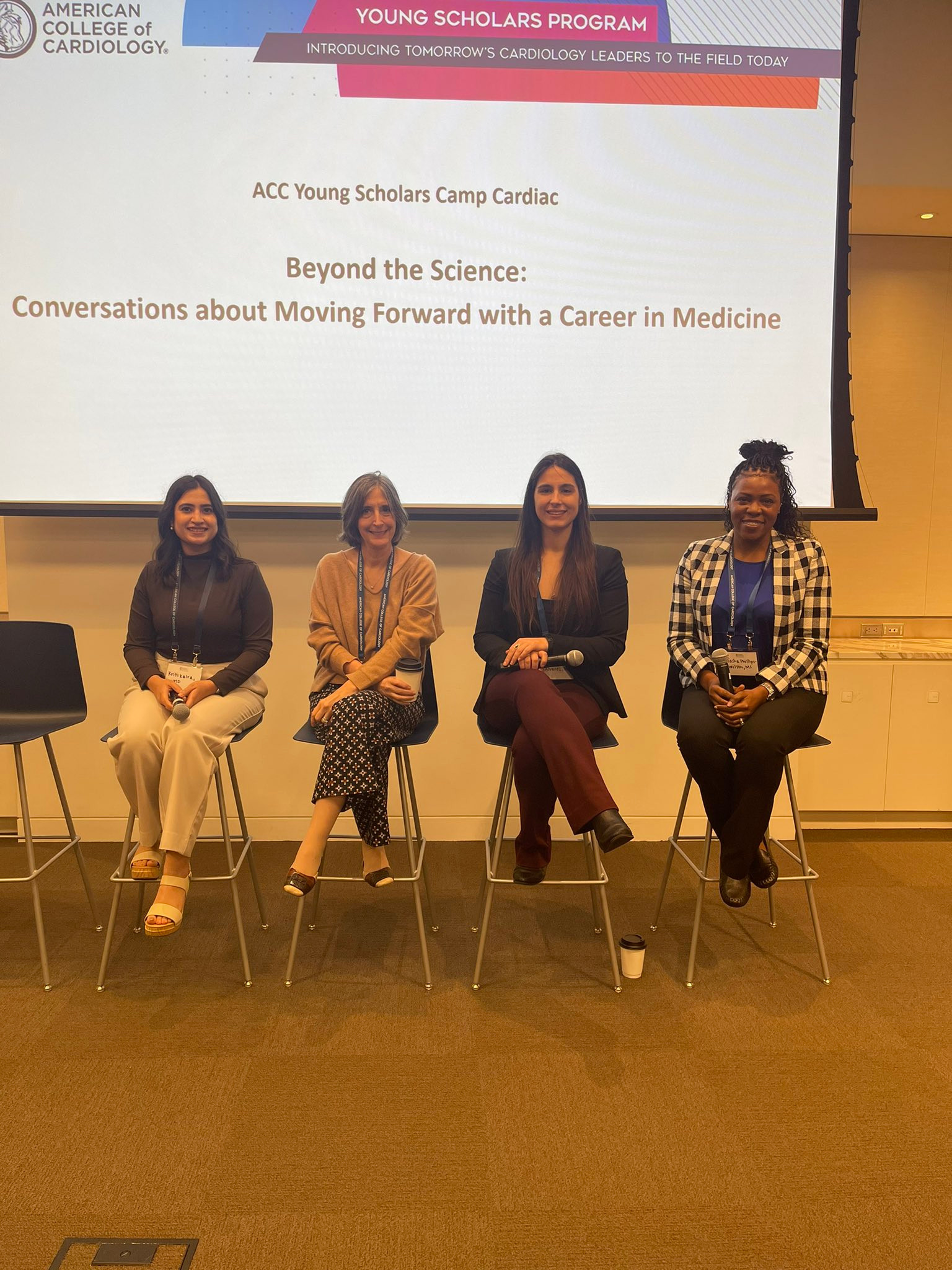 Dr. Melissa Alvarez (second from right) during the ACC Young Scholars Camp Cardiac presentation at the American College of Cardiology headquarters in Washington, D.C. Photo: Courtesy of Dr. Alvarez.
Dr. Melissa Alvarez (second from right) during the ACC Young Scholars Camp Cardiac presentation at the American College of Cardiology headquarters in Washington, D.C. Photo: Courtesy of Dr. Alvarez.
But I think the best part about where I did residency was that, over the years, you really did get more autonomy and you were able to make more decisions on your own and be watched more from the outside. Someone was checking on you, but you didn't necessarily know. They made it seem like you were completely in control. And I think that raised a lot of confidence because I was making decisions on my own. I had COVID-19 thrown in there during residency, so that put a knife in everything and made everything change pretty quickly. But at the end of the day, I think that was the best part, being able to make decisions on my own and feel like I was being given the opportunity to make decisions, sometimes make mistakes, and learn from them and grow that way.
 Dr. Melissa Alvarez at the UMHS White Coat Ceremony back in 2012 in St. Kitts. Photo: Courtesy of Dr. Alvarez.
Dr. Melissa Alvarez at the UMHS White Coat Ceremony back in 2012 in St. Kitts. Photo: Courtesy of Dr. Alvarez.
Why UMHS?
Getting back to your medical education, what made you decide on attending UMHS over other med schools?
I had an interesting pathway. I actually never applied to school in the United States. I only applied to Caribbean med schools. The reason why I ultimately chose UMHS was my interview. I'm originally from New Jersey, so UMHS headquarters in New York City was a very close train ride away. I went with my mother to the interview at headquarters in the city. And that interview was just so different than any other interview I had been on. I really felt like the administration really cared about you as an individual and not just your test scores and how you did academically. They asked a lot of questions about myself, my hobbies, why I wanted to do what I was doing, whereas a lot of other places focused more on grades and academic accomplishments, and I just felt that UMHS cared more about the overall person rather than just numbers and statistics. And that, for me, was very important.
I also knew of the fact that they had opened Ross and that was successful and there were successful graduates from there because back when I was interviewing, UMHS was fairly new. So, a lot of people had paused with that, but knowing that they had been successful previously, I didn't feel any hesitation. I also knew a current student who was there, and I talked to him and I was sold. Once I got accepted, I didn't hesitate to say yes.
 Dr. Melissa Alvarez on a hike in St. Kitts back in 2013 when she was a UMHS student. Photo: Courtesy of Dr. Alvarez.
Dr. Melissa Alvarez on a hike in St. Kitts back in 2013 when she was a UMHS student. Photo: Courtesy of Dr. Alvarez.
Is there anything specific about your medical education at UMHS that's really helped you accomplish your goals and become the doctor that you are today?
I think the greatest thing about UMHS is its professors. They are absolutely incredible people. They really want you to succeed and they really root for you. Their doors are always open. If you ever have a question, you can just walk into their office, shoot them an email, ask them in class.
The other great strength is the smaller class sizes, so you don't feel like a number. Your professors know you. The environment never felt like a place where people were competing. Everyone rallied around each other, would make study groups. Everyone roots for each other. We all want everybody to succeed. And I think that's a great strength because when everyone's lifting each other up, it makes everything a lot easier. Especially knowing that you're so far from your family and you can't go home and see your friends and everything, having an environment that is uplifting you is really great. But the professors put so much of their time and energy, you can tell that they all really love what they're doing and they all really genuinely want to be helping you and want to be there. It just made it so much easier to succeed knowing that I could go up to a teacher at any point and ask a question and it would be answered immediately.
Okay, great. And is there anything you'd like to say to those current prospective students out there, not only possibly considering UMHS, but looking at possibly a career in cardiology or internal medicine? I mean, what would you say to the current prospective students out there?
I would say that UMHS is definitely a great place to go if you're looking to grow, looking to learn. It really is a great place. The island itself is great, and in terms of internal medicine, there is such a great need for internal medicine physicians. You will have no problems finding a job. If you are someone who likes to make connections with patients and likes to have a relationship with patients, internal medicine is a great place to start. If you choose to specialize in anything, I'm partial, but cardiology is a great field. You can really make a difference in people's lives. You don't have to be someone who wants to do procedures in order to make that difference. There's a huge need for people in preventative cardiology and for heart failure specialists.
Again, cardiology is a specialty where you make connections with patients, and you see patients throughout their lives in completely different stages of their lives. You may see them one day in the emergency department having a heart attack and 10 years later you're talking about how they're getting married and having kids or having grandkids. So, you get that longevity with patients and you also get to make an immediate impact.
I think the heart is the best organ physiologically to study. It just makes sense. There's that too, but you definitely get to make connections with people, which is a great thing in my opinion.
 Dr. Melissa Alvarez (second from left) at UMHS Graduation in New York City back in 2017 with her parents & family members. Photo: Courtesy of Dr. Alvarez.
Dr. Melissa Alvarez (second from left) at UMHS Graduation in New York City back in 2017 with her parents & family members. Photo: Courtesy of Dr. Alvarez.
Growing up in New Jersey
Dr. Alvarez, can you tell us a little bit about where you grew up and when you decided to become a doctor?
I grew up in New Jersey, in northern New Jersey—very close to New York City. I honestly don't know what exactly made me choose to be a doctor, which is funny. I was that child that loved going to my pediatrician's office. I would play with all of her equipment. It was really funny. It would be me playing with everything and my sister sobbing that she wanted to leave. And from the time I was a kid, I just always said I wanted to be a doctor. If you ask my parents, there has never been anything else I've ever said I wanted to do. And my trajectory has never changed, which is strange. But I've always just really loved science. I've always loved studying anatomy, and physiology. I always had little science kits as a kid, a little microscope, all that stuff. So, it's been a long road with no exact... There wasn't ever anything that made it click. It just naturally happened.
You attended Wagner College in Staten Island. And you earned your undergraduate degree in biology. What made you want to study biology?
It was funny because I was actually between majoring in biology or chemistry. And chemistry had more math, which deterred me from chemistry. But also, biology had more physiology, it had more anatomy stuff than chemistry did and I enjoyed that stuff. Obviously, there were other things I wasn't as interested in because with biology you learn about everything. It's not just human anatomy and physiology. You do plants. You do other animal physiology. But at the end of the day, I liked learning about the nitty-gritty of how our bodies are composed. I really love genetics. I like human biology. So those classes lead me towards biology rather than anything else.
I don't want people to think that that's what you need to major in because I've had friends... Actually, one of my mentors in my cardiology fellowship majored in English as an undergrad and just did the science courses in order to apply to med school. I think it's important that whatever you choose to major in, it's something that you enjoy. I happen to enjoy the sciences, so that's what I wanted to do, but I don't want people to think that that's the only road to get into medicine because it's not.
That’s a very important point because many undergrads think that they have to follow a pre-med track to qualify for med school. And what they don't realize is you can major in English or really anything as an undergrad—like, for example, Latin is also a great major if you're thinking of med school. As long as you take biology and chemistry and other prerequisite science courses, you can major in whatever you want.
Right. You have to take the required courses to get in. But I know history majors that have gone to med school, and English majors. You can major in anything. I'm pretty sure we had a chemical engineer in my UMHS class. So, you're not restricted to a certain pathway.

Dr. Melissa Alvarez in her parents' homeland of Cuba when she was doing volunteer work in healthcare. Photo: Courtesy of Dr. Alvarez.
Volunteer work in her parents' native Cuba
I see that you did some volunteer work in Cuba and other places. Why do you feel it's important for med students and also young doctors to give back, especially in medically underserved communities or developing countries?
I think it works two-fold. You are not only giving back to that community itself and helping people, which is something that if you're becoming a doctor, I really hope that that's one of the main reasons why you're doing it, but it also gives you a deeper appreciation for what you have and what is at your disposal. Being able to go to Cuba was great for me for two reasons. One, I like doing volunteer work and giving back, and having that opportunity was great. The second was that my parents were actually born in Cuba and I went to the city where my father was from, where he was born and raised. So that was great because I had a deeper connection. But being there, talking to the doctors there, talking to residents there, talking to patients there, we all have the same base of knowledge.
Medicine is the same everywhere. The difference is what is available to you and what tools you have. So, coming to the appreciation of when someone comes into the emergency department here, I'm not worried about if the hospital has in stock the medicine I want to give. I just order it and it's given. But in other places in the world, they have to sit and think, "Does my hospital have that medication? If they don't, what can I use?" And we're very lucky here in the US that we don't have to worry about those things. And I think sometimes that gets lost on you as you're in training because it's just what we know. And then you go somewhere else and you realize their training is no different than yours. They don't know any less than you do. They just have fewer resources. And so being able to see what they do with those resources sometimes makes you realize that they're able to do things differently because they don't have what we have.
Being able to give back to patients, they're always just so appreciative of your time of being listened to. And coming back to America and then trying to put out awareness that other places need help because they lack resources because they lack the equipment that we have. Sometimes they just don't learn the newer techniques because they don't have the supplies to do so, not because they don't have the knowledge or the ability. So being able to go there, we brought some equipment with us and we were able to teach them some new procedural techniques that they weren't aware of because of their lack of equipment. And then I got to see how sometimes they think on their feet and improvise. And that helped me be aware that if everything isn't perfect, you can still make the best of a situation. It was incredibly eye-opening and something... I've always really wanted to do Doctors Without Borders at some point. So, this is a sprinkling of what that would be like.
It must be amazing to go to a country like Cuba as opposed to the USA. I think the pharmaceutical companies here have so much power and influence in this country. I mean, all the TV ads that we have in America, with so many meds available, and in other countries, they don’t even have pharma ads.
Which is so funny because I go to conferences and that's one of the things that's commented on. In other countries, there aren't ads for medicines, but they come here to our conferences and they're like, we can't believe that you advertise for everything on TV. That's absolutely crazy that a patient can come to your office and be like, "I want this med." That's just not how it is in other places. And it's eye-opening to see the differences and the good and bad of those differences.
 Dr. Melissa Alvarez in PPE at a hospital during the midst of the COVID-19 pandemic. Photo: Courtesy of Dr. Alvarez.
Dr. Melissa Alvarez in PPE at a hospital during the midst of the COVID-19 pandemic. Photo: Courtesy of Dr. Alvarez.
Lessons learned during pandemic
I really got to know you during the COVID-19 pandemic because we did a lot of features on frontline workers, and I know that you were working a lot during the COVID pandemic on the frontlines. What do you think you learned as a doctor during this unprecedented and very scary time in America? Not only for the general public but especially for healthcare workers and doctors?
That's a very good question. I think during that time, the uncertainty was difficult, but I think that I learned that you have to, as a physician, stick up for your patient. And when you think a patient needs something and deep down in your gut you know that what you want to do is the right thing to do, sometimes you have to advocate for that, even though it may be against protocol or it's not what's being done. Because especially during COVID, there were a lot of times when we didn't know what to do. No one knew what to do. So, everything that you were doing was scrutinized even further and more questioned because there weren't protocols for what we were doing. But I think at the end of the day, you know your patient, and so you need to advocate for what you think your patient needs to get so that your patient can get better and survive. I think that was one of the biggest things that I learned.
Another thing that I've learned is that you're not going to change a patient's mind about something. I think the biggest thing now is people asking me, "How do you deal with people who don't want to get the COVID vaccine?" [They] don't believe in it, and you just have to accept that you're not going to change that person's mind. All I can do is tell them the information and then they have to make the decision that's right for them. Whether I think it's the wrong decision or not, I have to respect that decision.
And it's very hard because we're trained. I've read the papers, you read the research, and you know that most—I'm not going to say all patients don't read the research because I'm sure there are some that do, but a lot of the times where people are getting information from is not the greatest source of information. So, you're struggling to fight against that, but at the end of the day, you just have to realize you give the information, you do what you can do, you advocate for them as much as you can, but at the end of the day, it's the patient's choice what they're going to do. It's their body. They're going to make that decision, and all I can do is educate as much as possible and hope that they trust that I'm giving them correct information.
It was a difficult lesson to learn because you get frustrated and sometimes you want to shake people and be like, "No, but please just listen to me," but you can't. So that was a tough lesson to learn, but it's been useful.
Why cardiology?
What interests you the most about the field of cardiology? You may have already answered some of this earlier.
I think cardiology is a great field because there's just so much that you can do and there are so many different ways you can go. If you're someone who's very into primary care and disease prevention and that realm, you can be a general cardiologist and do that and really make sure that your patients hopefully never get to the point where they need a procedure or anything like that. You're the person that's checking their cholesterol. You're making sure their blood pressure's good. You're basically their primary care physician for their cardiovascular system.
And then, within that, you can do a lot of other things. If you're someone who's really into MRI or CT, you can read cardiac MRIs. You can read cardiac CTs and perform those. You can be a specialist in echo and do 3D echo, TEEs, do structural TEEs if you're someone who really likes imaging or that aspect of procedures. And then there are people that go into procedural specialties.
And in cardiology, it's not just interventional cardiology, but there's also electrophysiology where you're dealing with the electrical system of the heart and treating irregular heart rhythms and doing procedures like cryoablation where they're freezing parts of the heart to treat arrhythmias. There is sports cardiology for people who are really into athletes and making sure that they are physically fit enough and their heart is well enough to do sports. There's just such a wide range of things that you can do that I don't even think I knew when I chose the specialty. I really just chose the specialty because I enjoyed the actual physiology behind everything. And then, from there, it just went into this is all the things that you can do. But no matter what you choose, the fact that you make connections with people and see them for a long time was another thing that I really enjoyed about the whole specialty.
Each February, the American Heart Association devotes the whole month of February to Heart Health Month and raising awareness about heart disease, especially for women because one of the number one killers of women is cardiovascular disease. What should young doctors—and also just women in general—know about heart health and cardiovascular disease?
Cardiovascular disease is a disease that really doesn't discriminate. It doesn't care if you're young, if you're old, what nationality you are. It really doesn't matter. It affects everyone. And I think the biggest thing with cardiovascular disease is that you can have it and feel absolutely fine. You can have high blood pressure and not know it because you don't necessarily have any symptoms from it. You can have high cholesterol and not know it because there really may not be any symptoms until you're having a heart attack. I think the really important thing is that you need to have a primary care physician. I feel like most people don't, and I know most people in my age range—even people I train with—don't go to primary care doctors. And you really need to know your numbers. You need to know what your blood pressure is. You need to know what your cholesterol is because if you don't know, you can't fix it and you can't be ahead of it.
People also need to be more active in their lifestyle, especially now with so many people working from home. People aren't moving, and that is going to be a real big problem later on down the line. It's recommended that people get at least 30 minutes of activity, at least five times a week, at a moderate intensity level. People assume that that means going to the gym, lifting weights, running on a treadmill. You can walk for 30 minutes a day and that will do wonders for you. And you don't have to do the 30 minutes all at one time. You can walk for 10 minutes three times a day, and that still counts. I think it's just very important that people get more active, that people see a primary care physician and are being proactive and taking care of themselves because I don't think that a lot of people do that.
I think there needs to be more proactiveness instead of reactiveness because if you're seeing a cardiologist in the emergency department, it's too late at that point. You can still make changes, but now you already have a problem. If we start now, if you're in your 20s and your 30s and get it under control, then hopefully later you won't have a problem.
It's also important to know your family history because people who have relatives who have had heart attacks at a young age or people who have passed suddenly at a young age are at a higher risk and should be getting screened earlier. It’s very important to talk to your relatives and know what's going on in their health as well so that you can be screened and you can be taken care of. It's a silent killer and it's called that because it doesn't have symptoms. It’s important to get checked, get screened, and know your numbers, the most important thing.
So, it's important for people to go see a primary care doctor at least a couple of times a year, have blood work done, have their cholesterol checked, their A1c, their blood pressure, all of that.
Exactly. You want to have everything under control because it's all interconnected. If you have diabetes, you're at higher risk for cardiovascular disease. If you're overweight, you're more at risk for cardiovascular disease. If you live a sedentary lifestyle and are at a good weight, you're still at higher risk for cardiovascular disease. So, knowing your numbers, trying to get some physical activity in. Diet is also important. Trying to eat as healthily as possible, staying away from eating a ton of red meat and a ton of carbs. It's a whole holistic picture. There isn't one thing that's going to completely reduce your risk to zero, but if you try to take care of the whole picture, your risk is going to go down.
You have also worked as a clinical instructor at the Robert Larner, MD College of Medicine at the University of Vermont. Is there anything that you'd like to say about your work there?
Through our cardiology fellowship, all the fellows are considered clinical instructors at the University of Vermont School of Medicine. The University of Vermont School of Medicine actually sends their med student. They have a campus, a clinical campus at Danbury Hospital. You have the choice when you study there to do your rotations in Vermont or to come to Danbury and do your rotations. So as a clinical instructor, what that means is we give weekly sessions to the medical students on EKG reading. So once a week, whichever, it's usually about a group of three or four of their med students. And we teach them about EKGs, teach them about different arrhythmias, and how you can tell what it is on an EKG versus telemetry. And it's a good way for us to keep our knowledge base up and to teach ourselves too because, at the end of the day, I need to know this information too. So being able to teach that to a med student and explain it in a different way helps us learn as well. So yeah, it's been fun.
In cardiology, are there currently any cutting-edge treatments or new breakthroughs that are new and exciting that you want to talk about?
They're not super new, but I think the ablation techniques that the electrophysiologists have are just so incredibly interesting. Atrial fibrillation is an arrhythmia that is extremely common all over the world. And as people get older, the odds that you have that arrhythmia are increased just because of age. There are a lot of other risk factors, but in the past 10, 20 years or so, they've developed ways to go into the heart and burn or freeze it so that the arrhythmia doesn't happen, which just boggles my mind that you can go in there and just freeze a part of heart tissue and everything's fine.
The fact that we can do valve replacements and all that without having to open someone's chest is another thing that just boggles my mind that we're able to do that. And watching them always is like, what is happening? But I just think that everything that's being developed procedural-wise, it's just really exciting.
I think too, with things like ChatGPT and AI, it's just going to get even more [possible to do things at] a patient's bedside and do an echo on an iPad. My attendings would've never thought that they would be able to do that. So, it's going to be interesting to see, not just within cardiology, but in medicine in general, what happens with AI and everything. It's going to be very interesting
Do you want to give a shout-out to any of your favorite professors that you know are still at UMHS?
Dr. Purcell was one professor who was very near and dear to me. He was just great. He really cared about everybody. He's one of those people who still, when I have some accomplishment, is there messaging or commenting and watching and cheering on everyone's success. The other professor who was really great, he passed away, our neurology professor. That was a big blow, I think, when we all found out that he passed away because he was really great.
Are you talking about Dr. Michael Doherty?
Dr. Doherty—yes.
It was very sad when that happened.
He was great. His class was not necessarily a topic that I was extremely interested in, but every time you were in his class, he made it such that you thought it was the coolest thing. And he was just so engaging with everybody that he wasn't someone that just stood there and lectured. It was more interactive. So, it made it great. Dr. Mungli also.
Dr. Prakash Mungli, yes.
Yes. He was another one. So incredibly engaged. Tough, definitely tough, but he wanted what was best for you and he prepared you so incredibly well and set you up for success. I mean, that's just really the common theme of all the professors there. They just really wanted you to succeed. And at the end of the day, even if they were tougher or easier or however you wanted to phrase it, they just were trying to do their best to see you succeed. And that was just... I've nothing but great things to say about the professors there. They were just really great.
Is there anything you’d like to say to the alumni out there?
Well, at least when I was at UMHS, I think it's changed a little bit now, there weren't a ton of hubs where you could do all of your rotations in one place. You were moving around a lot, so everyone got lost in the shuffle, so to speak. There are people you just ended up losing touch with, not because of anything other than you're moving around, you're doing your own thing. So, it'd be really cool to get everybody in some way interacting again because I want to see what everyone's doing. That was the cool thing, was that, like I was saying earlier, there was never a huge environment of I need to be better than you at UMHS. Everyone was really into, "What are you struggling with? Let's start a study group. Let's figure this out. Let's all lift each other up." So, it'd be really great to see everybody and get everybody back together. And it's a good way to help the school grow too because having an Alumni network is always great in terms of getting mentorship or even being like, "Hey, I'm looking for a job. Does anyone know what's going on?" within us alumni.
I think it's a great thing. I would love to go back to St. Kitts and see what it looks like now because it seems like they've built so many resorts and done so many new things since I left. And the school, they have a basketball court now, all of this stuff. It would be cool to go back and see everything again.
Dr. Alvarez, is there anything else that you'd like to add that we haven't covered today?
I am just thankful that I was able to attend UMHS and I was able to achieve what I was able to achieve. Everyone there, the professors that I still am in communication with on social media, they're still celebrating our successes even when we're long gone. I graduated in 2017 and there are still professors that follow me on Facebook. And anytime that I've met a new milestone, they're messaging me and encouraging me. So, the relationships don't end once you graduate. The UMHS Alumni; it's an amazing community and I want to thank the school for giving me the opportunity today to even talk. I really appreciate it.
Contact Dr. Melissa Alvarez via LinkedIn.
(Top photo): Dr. Melissa Alvarez. Photo: Courtesy of Dr. Alvarez.

Scott is Director of Digital Content & Alumni Communications Liaison at UMHS and editor of the UMHS Endeavour blog. When he's not writing about UMHS students, faculty, events, public health, alumni and UMHS research, he writes and edits Broadway theater reviews for a website he publishes in New York City, StageZine.com.