UMHS Class of 2022 graduate Dr. Alexander Khobeir started an Emergency Medicine residency at McLaren Oakland Hospital in downtown Pontiac, Michigan in the summer of 2022. He is currently a PGY2 resident.
Dr. Khobeir spoke to the UMHS Endeavour on a break from his busy day of working in the ER in Michigan. He is currently in his second year of residency at McLaren Oakland Hospital, serving a medically underserved area of Michigan. He first heard about UMHS from Corie Helms Thayer, Associate Director of Admissions–Midwest.
Why UMHS?
UMHS Endeavour: What made you decide to attend UMHS? I understand that you and your brother both transferred from different med schools and that you graduated from UMHS, while your brother is currently a present student at UMHS. Correct?
Yes. My story is quite tumultuous. I endured Hurricane Maria while I was a medical student in another university at the time. We went through the cruise ship, and unfortunately the resources that I needed to get to where I'm at today I could not be provided with. I've only heard great things about UMHS prior to even thinking about transferring. I know that [part of] the family is Michigan-based, and that is actually at the time where I had my interview and talked with many, many staff at the time.
You have a really great working relationship with Corie Thayer in admissions. Can you tell us a little bit about what that experience was like with Corie?
Corie was the first person I met in Michigan. UMHS has an office in one of the cities near where I live, and I ended up going to an interview. I remember Corie at the time was not in the position she is now, and she introduced herself. She was super nice. Very calming. I went there for an interview at the time and I had so many questions. I had never transferred in my life and it was a great experience. I think overall I had no problems whatsoever. Any questions that I had, anyone and everyone would answer. I usually got more than one answer, and they were really consistent, and I was really happy with that. They—Corie especially—put me in touch with different alumni, different current students that I could talk to when I was transferring, but my mind was pretty set on transferring here at the time because of the great Ross family relationship that I had heard of, and the former school being a Ross school as well.
Can you tell us one or two things about UMHS that really helped you become the doctor that you are today?
I cannot thank the fifth semester enough. I transferred into the Maine fifth semester, and it was really the fifth semester that did two things. It gave me the clinical knowledge and it gave me the ability to talk with the doctors where I'm at now. It allowed me to have the sense of ease that I could do this once I was in the real hospital setting. And the other part was of course passing my boards. At the time I needed to take Step 1, as everyone does, and UMHS provided me with the opportunity to take a course during the fifth semester Maine. That, including Dr. Thibodeau, who was the program director in fifth semester Maine, was great. That allowed me to do everything I needed to be where I'm at now.
 Dr. Alexander Khobeir (center) with friends at 2022 Graduation at Lincoln Center, NYC. Photo courtesy of Dr. Khobeir.
Dr. Alexander Khobeir (center) with friends at 2022 Graduation at Lincoln Center, NYC. Photo courtesy of Dr. Khobeir.
What would you say to a current or prospective UMHS student who's thinking about not only going to UMHS, but also going into emergency medicine? What's some advice you would give them?
One of two things. Either way, it's going to hopefully end up with the same thing. First, come have a conversation with me. I have no problem. I will give you my phone number, we can talk, we can Zoom, we can meet in person when I have time off. But any specialty that you're going to—not just specifically emergency medicine—the road is long. So, for any prospective student, you need to understand that. It's okay, it's going to be hard. Make sure you have a good support system. Make sure that you are able to get that support system at any time if you need to get in contact with them. You can always call me for support.
The second part is, emergency medicine alone, there's a big difference in the acuity, I would say. It is fun, for sure. It's very exciting. But at the same time, you have to be able to think on your feet, and it's not all the time, but when you do, you have to be quick about it, because it's a person's life.
It is very rewarding. That's something that I tell students all the time. Emergency medicine is not for everyone and that's okay. At the same time, you are going to learn a lot, and that's in any area of medicine, but especially emergency medicine. You're going to learn to work through a lot, because you are balancing more than one patient at one time. You are managing higher acuity patients, and you never know what's going to happen. You don't know what's going to walk in through that door. So be really mindful about what you want to go into and think about your own strengths. You have to sit down and really have that inner conversation with yourself about “what can I do and what can I not do”? And it's hard in the beginning because you don't know. Make sure you do your rotation emergency medicine, have conversations with people, and at the end of the day, just have fun.
Is there anything else that you'd like to say to current or prospective UMHS students?
The most important thing is be realistic with yourself, have a good support system, and know that this is not a sprint; this is a long journey. Don't burn yourself out. Have fun along the way. The end is going to be there no matter what you do, so relax a little bit. It's going to be hard, but take it one step at a time and I promise you'll get there.
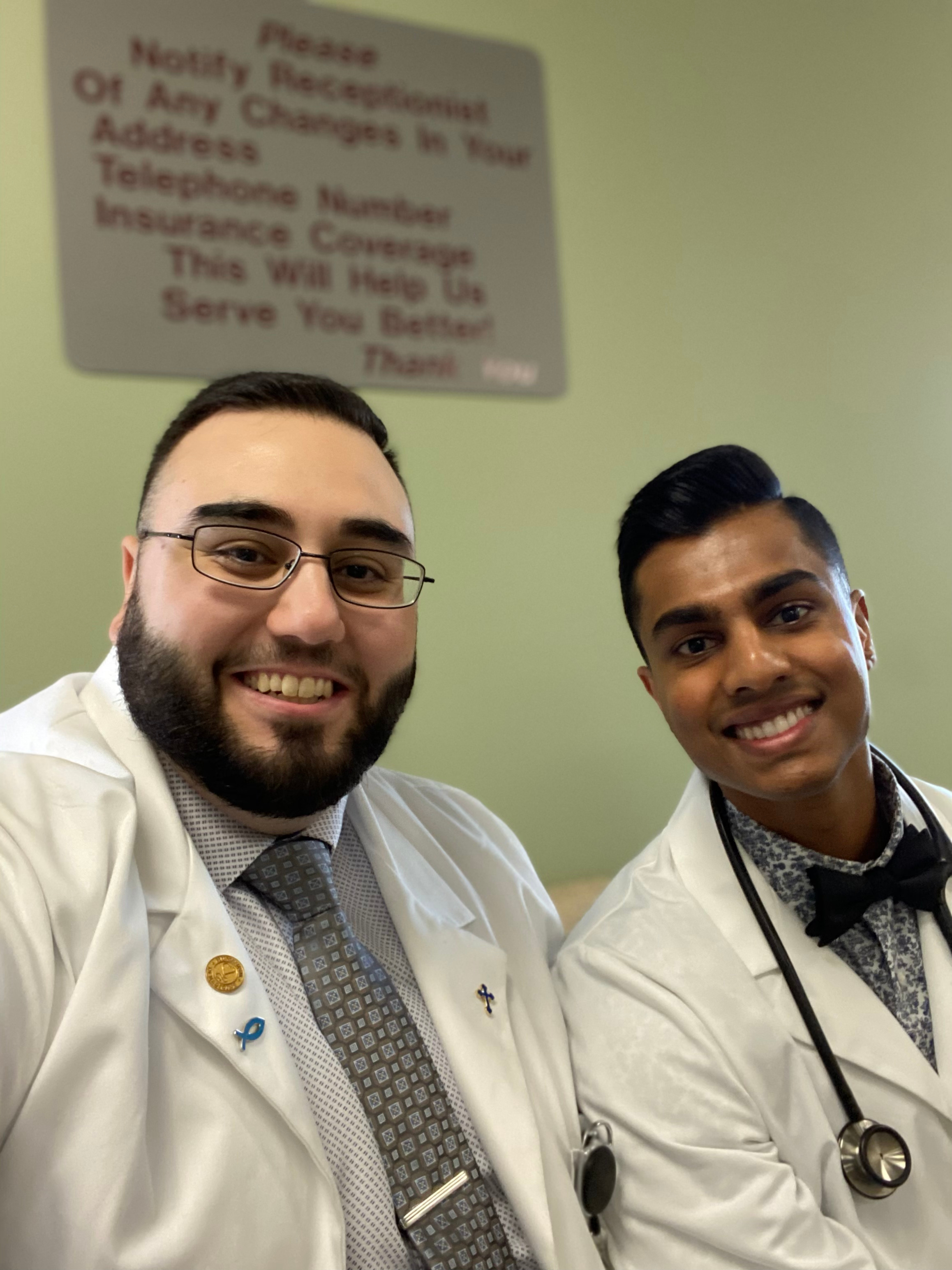 Dr. Alexander Khobeir with fellow UMHS grad Dr. John Abraham. Photo courtesy of Dr. Khobeir.
Dr. Alexander Khobeir with fellow UMHS grad Dr. John Abraham. Photo courtesy of Dr. Khobeir.
Growing up in Michigan
Dr. Khobeir, where did you grow up and where did you do your undergrad?
I lived in La Salle, Michigan. It's a small town about 10 miles north of the Ohio-Michigan border. I grew up there basically, until I went to college. I went to the University of Michigan. I obtained an undergraduate in biochemistry and another degree in molecular biology, biotechnology. At the time I was not satisfied with the education, so I also obtained a master's in biochemistry. I was contemplating whether I wanted to do just an MD or an MD PhD. at the time. So that's one of the reasons why I went and got my master's, in terms of the research. To this day I still love both. So, yeah. Being a doctor was always my goal. In terms of what field, it was really hard. I contemplated getting a PhD in clinical biochemistry, so I would not be a medical doctor, but I would be in terms of consultation for genetic diseases, terms of treatment, being liaison between pharmaceutical companies and current medical doctors. I also wanted to go into biotech to build different medical devices. I think at the end of the day, what really set the difference for me was the interaction with the people. I needed interaction with people. I didn't want to just work in a lab. Having that relationship is more important to me. I always grew up fostering a relationship from basically nothing. From, "Hey, how are you?" to knowing a lot about you.
What is Emergency Medicine?
Could you explain a little, especially to prospective students that may not know, exactly what emergency medicine is?
Absolutely. Emergency medicine is, I think, one area of medicine where you have to use everything. I'm talking from psychiatry, to internal medicine, to pediatrics, to family medicine, to surgery, to OB-GYN. Emergency medicine, foundationally, is about treating medical emergencies. Unfortunately, or fortunately, depending on how you look at the system now, it is not that anymore. It's also a lot of primary care, we'll say, but it's not a primary care. It's, "I need medical attention now. I need this doctor to quickly figure out what's going on and take care of that."
I would imagine, with emergency rooms, it's everything from people that were in car accidents, to life-or-death situations. So, people that might have something like undiagnosed diabetes, or, you name it, that they would have some kind of emergency. So, it's not just the trauma, I would imagine, you're saying; it's also people that maybe have underlying conditions that they haven't had properly diagnosed. I know a lot of people don't like to go to the doctor until it's an emergency, so I'd imagine it's a lot of that?
Yes. The TV show version of emergency medicine, which is the car accidents and the gunshots and the stabbings, I would say that that's maybe 15% of emergency medicine. Do you see it? Yeah, absolutely. Everyone has their story. Everyone has the situation that they've been in. But it is a lot, especially depending on where you practice. Obviously, I love working in this. Prior to this I worked in Genesee County in an underserved area in Flint, and now I'm in Pontiac in an underserved area.
It is exactly like you said, Scott. It is a lot of people who just don't have access to healthcare even if they wanted to. They are presenting to the emergency department for the medical emergency of diabetes, which is diabetic ketoacidosis, which is incredibly life-threatening.
It is unfortunate, and I think that it's not as showy as the traumas and the gunshots and everything, but I think it's probably more important in terms of the social economic aspect of medicine. You see, you're first line. You have to figure out where can I get this person to give them the best help, the best access to medicine outside of me taking care of them in an acute setting? It's incredibly hard, but thankfully we have a lot of resources here, in terms of free clinics, in terms of working with pharmacies. And social workers. I cannot tell you how many times I have called over, for example, even for alcoholism, to get them to a place where they can get the help they need.
 Dr. Alexander Khobeir out with friends. Photo courtesy of Dr. Khobeir.
Dr. Alexander Khobeir out with friends. Photo courtesy of Dr. Khobeir.
A typical day for an Emergency Medicine resident
What would a typical day be like for you? What does a typical, normal every day that's... just to give people an idea of what you do?
Emergency medicine is “shift” work. What that means is you have your schedule a month in advance. As a first year, you usually work about 20 10-hour shifts. As a second year, you'll work 19. And then as a third year, you'll work 18 shifts a month. And those are, again, 10-hour shifts. There are six different shifts in a day. So, you have a lot of what we call coverage, or people to help you. You also have supervising attendings, which, at our hospital, they are very hands off. They want you to learn. That is the whole point in their eyes.
So, you would come in, let's say, at 9:00 in the morning. You would pick up patients. You would go see patients. You would make sure that you have the proper workup in terms of talking with the supervising attending, "Hey, this is what I'm doing. This is why I'm doing it. This is what I think they have." And they're going to ask you, and then they're going to teach you. "Hey, these are the mistakes you made. This is what I would've done. But I understand why you're doing this, and this is how you can become more efficient." Which is, of course, always important, because efficiency also has everything to do with saving people's lives. Because if you start stacking up patients, then something really big comes in, you're not going to have time to manage everything. So, you have to be really efficient with your time.
So, once you come in, you see your patients, you write your notes, you're able to go home. Let's say that a workup wasn't complete because there's a CT scan, and there's also 20 ahead of that person. That's okay. What we do, we would sign out to the new oncoming resident and they would take over management. So, it is a really beautiful teamwork aspect of medicine in emergency medicine. And you have to be really good with communication and relationship building, and again, just being open and saying, "Hey, did I make a mistake here? Where can I improve?" Feedback is also incredibly important.
What do you like the most about emergency medicine? What are some of the most rewarding aspects of this specialty?
There are two, and it's the one that almost everyone goes into emergency medicine for, the trauma. We call them trauma aspects. It's rewarding because you know doing X gives you an immediate reward. You see this person coming alive. You see his color change giving him blood.
The other aspect is the socioeconomic aspect. When you have, we call it disposition. It's where we get this person, this human being to a place where they can get the proper treatment long term. It's incredibly rewarding to me to be able to pick up the phone, make that phone call, have a relationship on the other side, have that doctor professional relationship, and say, "Hey, I have a human being here. This isn't just a patient. They need help. I can only do so much. They are medically cleared, but they need long-term help. They need somebody to talk to in terms of a psychiatrist. They want to be sober." I think that's a really big complaint that we get in the ED. "I have this patient who really does not know what to eat for... and she's a diabetic. She can't afford insulin. Let's get in touch with a pharmacy to make sure that we can get them the medication they need." It's incredibly rewarding from that aspect. And those are also the two most enjoyable parts of emergency medicine to me.
What are some of the biggest challenges in emergency medicine and how do you deal with those?
There are two things that always come to mind for this type of question. The first one is failure, and the second one is doing nothing. So, what do I mean by that? Failure. You could do 100 things, and you have to accept that sometimes you can't do anything about it. You can't get this person here. There is no medication for this disease. There is only pain medication, for example, for this patient's cancer, for this person's cancer. There is no surgery that is going to cure this person of their ailment. They have sustained injuries in a trauma past what I can repair, or a surgeon, or this multidisciplinary approach to patients. You have to be okay with that. The unfortunate part is, yes, patients die. People die. But you have to say, "Did I do everything I could to make sure that I gave them the best chance?"
The second part is emergency medicine doctors always want to do something. Somebody comes in, you want to do something. Or you may do something and you don't wait long enough for the result. So, in some aspects, wait. Just hold on. Don't do anything more. And that really develops over time with experience and knowledge, that there are certain things that, yes, you can wait, and other things like, nope, you can't wait. I think those are the two most difficult parts of emergency medicine.
I think that sounds very challenging, understanding that sometimes people are going to unfortunately pass away or there's not much you can do for them. I think that's probably one of the hardest things of being any sort of doctor, is that when a patient reaches that point that there's really nothing that can be done. Having said that, what are some of the cutting-edge treatments that are now available in emergency medicine, or things that have emerged really since you've started that are exciting that you can talk about?
Usually these are in terms of procedures, life-saving procedures, or they are procedures that are done in an effort to save this person. I wouldn't say they are really new, as much as they are more improved, we'll say. For example, a central line kit, or a cricothyrotomy kit, where they have to cut when there's facial trauma. Intubation material, such as using a video to make sure that you are where you need to be. Or when there is a gunshot and I have to stop the bleeding, so I have to put in what we call a REBOA [resuscitative endovascular balloon occlusion of the aorta] to stop that bleeding.
In terms of very specific areas of emergency medicine such as eye care, having the equipment to measure pressures within the eye to make sure that there isn't increased pressure within the brain. Having specific stains to look at things. Having even something as simple as a bed. The stretcher that the patient is on. Those are new every day. These are becoming more electronic; they're becoming more technology-driven in terms of getting an image very fast. In the past we used to have to roll the patient over, put a board underneath them to take an X-ray. Now we don't have to do any of that. The board just goes under the bed and it takes a beautiful X-ray. In terms of machinery, for example, ultrasound.
We are incredibly, incredibly lucky. We have a program director and the emergency director who work together to obtain new equipment. We were able to obtain almost $100,000 in just brand-new ultrasound equipment. And we're trained on these to see what we need to see without costing the patient tens of thousands of dollars in terms of CT scans.
With that said, CT scans, MRIs, these technologies are continually improving, and I thank God that McLaren is the type of hospital that cares for its patients and they will buy new equipment. We don't have to wait for 100 years, for example, on something that's old.
In terms of buildings, whole infrastructures, there's talks right now in getting approved for a brand-new emergency department at McLaren Oakland. So, there is a lot. A lot. It's both directly and indirectly, but they're both affecting patients positively. Giving them the environment to be cared in and giving us the equipment to care for them.
Is there anything that you would like the alumni to know about, whether new alumni, or former classmates, or older alumni? Anything that you'd like to say to the UMHS alumni?
Thank you for being there, for support. I speak to prospective students. Adults who are thinking about medicine that are unsure where they want to go. People who are even in second careers as medicine. I see a lot of them when I'm sitting on boards to have a conversation with them. I've also had very amazing discussions randomly. “I didn't know you were a UMHS alumni,” for example.
At different events, when you're going to conferences, there are a lot of us, and we are in a lot of areas of medicine, from interventional radiology, to psychiatry, to family medicine. There is a lot. I think it's becoming more and more normal, I will say, for UMHS, as well as IMG grads, to hold positions that are influential to other people. I think that those that are in those positions are doing an amazing job and giving opportunities to everyone, being fair. I just want to thank them for that.
One last thing. You have a younger brother. Is he presently a UMHS student?
Yes. When I was coming home, Antoine, my brother was going into medicine. We were in two very different areas in terms of geography, and so we would always talk on the phone. At the time I think Antoine had started medical school, I was still at my former institution, and he had gone to a different institution, St. George's. Again, it's all about resources, in my mind. Not to talk badly about anybody, it's per person driven. It's not like an institution. But I truly believe that UMHS strives for a student-based approach to medicine, a per person approach. So, they really truly believe that everyone is different and they will get you the resources that you need. And I think once my brother saw that, once I transferred and I graduated, he was like, "Wow. What was I doing?" And once he got here, and now he's completing Maine, it was two different worlds, especially for him. It went from a “I'm a number” type of institution, to, "Oh, you're Antoine. Oh, I think I know your brother, too." They've always stressed this, but UMHS is incredibly family-oriented
UMHS truly is.
UMHS does for us what they would do for their own children. It’s great.
Contact Dr. Alexander Khobeir at akhobeirmd@gmail.com
(Top photo): Dr. Alexander Khobeir. Photo courtesy of Dr. Khobeir.
UMHS YouTube interview with Dr. Alexander Khobeir

Scott is Director of Digital Content & Alumni Communications Liaison at UMHS and editor of the UMHS Endeavour blog. When he's not writing about UMHS students, faculty, events, public health, alumni and UMHS research, he writes and edits Broadway theater reviews for a website he publishes in New York City, StageZine.com.