During the worldwide crisis of the COVID-19 pandemic, the UMHS Endeavour is interviewing UMHS graduates for our series “Alumni On the Front Lines.” For our third installment, we spoke to UMHS 2019 graduate Dr. Robertino Simpson, a surgery resident at the University of Florida Health hospitals, alternating between the Shands and VA (Veterans Administration) Hospitals in Gainesville, Florida.
Florida made the news the past week when Governor Roy DeSantis said anyone traveling via air from New York, New Jersey and Connecticut airports must self-quarantine for 14 days. Governor DeSantis was also criticized for not having a statewide order to close all Florida beaches during spring break.
The UMHS Endeavour spoke to Dr. Simpson about how his hospital is coping with COVID-19 and how the pandemic has affected his surgery residency, the need for COVID-19 tests, treatment methods, and his thoughts on why people need to stay home.

Dr. Robertino Simpson. Photo: Courtesy of Dr. Simpson
What’s Happening in Florida Now?
Dr. Simpson is in a University of Florida surgery residency that is a government program and he has had to do rotations at the Shands and VA hospitals in Gainesville.
“As of today, they have started to place us into cohorts (three groups); they have pulled me from the VA and as of tonight I’ll be on trauma/ acute care/burn as a part of the first cohort. This is an effort to prevent residents from being infected and sick in masses,” he said.
We asked Dr. Simpson to tell us how the COVID-19 pandemic is affecting the hospitals in which he works and the medical world in general.
“The incidence of COVID-19 rising globally has marked an unprecedented era in healthcare here in the US. Hospital management are faced with a crisis never seen before. Presently Medical students in clinical years have been removed from clinical rotations, non-essential staff have been told to stay home.
“As a surgery resident we now have to define what surgeries are important to undertake,” Dr. Simpson said. “In Florida, the governor has mandated the elimination of elective surgeries. This, I think, is a great move as it limits traffic of people. Most people have become familiar with the term “flatten the curve” which simplified means that less exposure leads to decreased incidence and spread of the disease. Stay at home!”
Everyone at the hospital is taking extra precautions.
“COVID-19 is transferred via respiratory droplets. Here at the University of Florida, all staff have been encouraged to get fit testing for the N-95 mask, we use droplet precautions on suspected patients utilizing PPE (masks, gloves, gowns).”
He said patients entering the VA and Shands Hospitals are screened at the entrance with questions assessing potential for high-risk exposure. The facility is minimizing patient contact by limiting the number of visitors and non-essential interactions.
Elective surgeries have been canceled and some follow-up appointments are being done over the phone.
“We are also increasing the number of screening tests for COVID-19 for both patients and house staff alike,” he said.
For now, Dr. Simpson has not had any direct interactions with a COVID-19 patient of which he is aware.
“I use standard precautions with all patients. I personally have refrained from excessive handshaking. I wash my hands between patients, which is standard, but in light of COVID-19, I think most people are more aware. As a surgery resident, many times I see patients in the ED, presently they are being screened for high-risk exposure and increased precautions would be implemented upon seeing them. The same stands for in-house consultations.
“Presently, COVID -19 has an incubation period of up to 14 days. Symptoms include shortness of breath, fevers, chest pains along with rhinorrhea. Initial symptoms can include a dry cough that progresses to shortness of breath and chest pain. On screening patients should be questioned about recent travel to endemic areas, and contact with high-risk individuals.”
Many large cities are building makeshift hospitals in convention centers and hotels but Gainesville, Florida has not yet implemented such plans.
Alachua County (where Gainesville is located) has 45 diagnosed cases, and the State of Florida has close to 2,000 confirmed COVID-19 cases as of UMHS Endeavour press time on March 26, 2020.
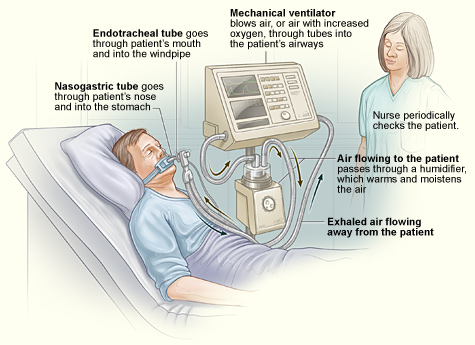 Illustration of a standard setup for a ventilator in a hospital room. The ventilator pushes warm, moist air (or air with increased oxygen) to the patient. Exhaled air flows away from the patient. Image: National Heart, Lung and Blood Institute (NIH)/Wikimedia Commons.
Illustration of a standard setup for a ventilator in a hospital room. The ventilator pushes warm, moist air (or air with increased oxygen) to the patient. Exhaled air flows away from the patient. Image: National Heart, Lung and Blood Institute (NIH)/Wikimedia Commons.
He said his hospital currently has a good supply of PPE, but this could change as needs rise. Ventilators are needed, however.
“Ventilation is one of the many supportive measures that are needed for the management of severe cases of COVID-19.” Dr. Simpson said. “The state of Florida has a vastly growing elderly population. With 23% of population over the age of 60, this could potentially lead to more severe cases in the future."
Should All COVID-19 Patients Be Admitted to Hospitals?
Do patients with confirmed or suspected COVID-19 need to be admitted to the hospital? What facts do doctors need to know?
“The vast majority of patients demonstrate signs and symptoms that do no necessitate hospital admission, and these patients can recover after symptomatic treatment and home quarantine from other individuals. Patients who develop severe respiratory symptoms characterized by worsening shortness of breath, inability to clear secretions, wheezing, and chest tightness and pain, and dehydration, despite conservative treatment at home and require hospital admission for further respiratory support.
How long do critically ill patients need to be hospitalized with COVID-19 and what types of health improvements are needed for a patient to be discharged?
“The length of admission varies greatly on the severity of the illness and the patient’s ability to adequately fight it. Patients without underlying complications who are able to recover respiratory function and breath without respiratory support can be discharged after three negative tests, which are spread apart by a period of 24-48hrs. In general, this amounts to a period of 1-2 weeks. Patients with severe symptoms, including secondary bacterial pneumonia and sepsis, leading to intubation and mechanical ventilation, require an even more prolonged course of several weeks. Once these patients can recover respiratory function to the level mentioned above, then they can be safely discharged home."
We asked Dr. Simpson to talk about supportive treatments for COVID-19 patients who may have complications like respiratory failure, septic shock and organ failure.
“Patients with severe complications generally experience multi-organ dysfunction involving lungs, heart, kidneys, liver, and other organs,” he said. “Initial management is generally increasing ventilatory support, but if a secondary infection develops then treatment becomes much more complex based on the type of infection and response to treatments. If these infection results in septic shock and organ failure, then priority becomes resuscitation focused on preserving vital organs (heart, lung, brain, kidneys) and success depends on how early on we can catch and correct these issues in context of the patient’s other comorbid complications.”
What about people with milder cases of COVID-19? What are some ways they are being treated?
“Symptomatic treatment (IV fluid hydration, respiratory therapy) if hospitalized. Others are sent home and told to self-quarantine. This, I believe, is ultimately the best way to minimize the effects of this outbreak.”
Why Everyone Must Stay Home
Dr. Simpson has a cautionary message for everyone.
“Stay home,” he said. “This cannot be said enough. This is our ultimate test as a global community. There will be many of us who are asymptomatic and still be out and about. This puts people who are vulnerable (those who have pre-existing lung issues) at risk of having a devastating life-threatening illness. Therefore, the only way to prevent this is to enforce and limit transmission by self-isolating.
“You can be present in your loved ones’ lives without being present. With the advent of social media, many turn to comedy to lighten the effects of this outbreak, I encourage this. Social distancing while necessary for decreased transmission, can have mental and emotional impacts. So, use this time to check up on family, friends via cellphone, Skype and Facetime. Maintain your relationships through alternative measures. I implore all of you to encourage family and friends to practice social distancing and self-isolation as best as they can.”
He offered examples of social distancing that allow you to avoid larger crowds or crowded spaces, such as:
- Working from home instead of at the office.
- Closing schools or switching to online classes.
- Visiting loved ones by electronic devices instead of in person.
- Canceling or postponing conferences and large meetings.
Self-quarantine involves:
- Staying at home.
- Using standard hygiene and washing hands frequently.
- Not sharing things like towels and utensils.
- Not having visitors.
- Staying at least six feet away from other people in your household.
Finally, Dr. Simpson quoted German writer and statesman Johann Wolfgang von Goethe, “Common sense is the genius of humanity,” and again urges everyone to stay home.
The UMHS Endeavour and UMHS website will be updated in the coming days as news of the pandemic unfolds.
(Top photo) Dr. Robertino Simpson (2019 UMHS grad) is currently working on a surgery residency at the University of Florida in Gainesville. Photo: Courtesy of Dr. Simpson
About UMHS:
Built in the tradition of the best U.S. universities, the University of Medicine and Health Sciences focuses on individual student attention, maintaining small class sizes and recruiting high-quality faculty. We call this unique approach, “personalized medical education,” and it’s what has led to our unprecedented 96% student retention rate, and outstanding residency placements across the USA and Canada.

Scott is Director of Digital Content & Alumni Communications Liaison at UMHS and editor of the UMHS Endeavour blog. When he's not writing about UMHS students, faculty, events, public health, alumni and UMHS research, he writes and edits Broadway theater reviews for a website he publishes in New York City, StageZine.com.
















