UMHS third-year student Jared Sharza was, like many, disappointed when his clinical rotations were abruptly suspended in Detroit due to the COVID-19 pandemic. So, he drove home from Michigan to Upstate New York, thinking, “I refuse to be sidelined.” While driving through Canada on the way back to New York, he was rehired by an EMS agency for which he had previously worked. He is one of the many medical students on the front lines of the COVID-19 crisis.
The UMHS Endeavour spoke to Mr. Sharza about what’s it is like working on the front lines of the COVID-19 pandemic as a first responder, the need for students at North American and Caribbean medical schools to work in hospitals during this crisis, six ways med students can help, and more.
‘I Refuse to Be Sidelined’
Mr. Sharza kept thinking something as he drove home from his canceled clinical rotations.
“ ‘I refuse to be sidelined,’ I kept frustratingly thinking to myself as I drove home from Michigan to Upstate NY,” he said. "I was flustered because, earlier that day, I had found out that my third-year clinical rotations were to be suspended due to the coronavirus beginning to increase in severity. I was less than two weeks away from completing my three-month internal medicine core rotation, and was scheduled to take my NBME shelf exam the day after I finished. I had been working diligently throughout the rotation with hopes of high marks on my shelf and a complete set of evaluations that would serve as quality referrals in the future. As I continued to drive toward home, I began to realize that this coronavirus would serve as an unfortunate opportunity to actualize my skills and education, an opportunity that is hard to come by when balancing a clinical schedule and studying. I came to terms that my frustration and self-pity would not help me persevere. These were reflex emotions I was feeling, that I’m sure the vast majority of medical students have felt at least once during the past few weeks. Nevertheless, I would refuse to be sidelined."

UMHS student Jared Sharza in PPE about to enter the ICU for a long shift. Photo: Courtesy of Jared Sharza.
New York State currently has the highest number of confirmed COVID-19 cases in the USA, with nearly 74,227 cases as of April 1, 2020, according to the CDC (Centers for Disease Control and Prevention). The total number of U.S. cases is 186, 101 and 3.603 deaths.
“These numbers will change, and have continued to change sharply each day,” Mr. Sharza said. “For me, it was a feeling of duty to return home and help in a medical capacity. I’ve remained an active member of EMS for six years and have been a NY-certified EMT for three years with a recent renewal for another three years. I knew that, going home, I would be able to help out immediately on the front lines. I let some of my friends, who work at my home agency, know that I was returning home in case they could use my help. While driving through Canada (it saves two hours on my trip), my EMS Chief called me and inquired about my return and indicated that he could use me immediately. We discussed re-hiring me as a per diem medic, and I started working the day after I returned home. Due to being short-staffed, I have worked every single day since being home. My passion for EMS, along with my commitment to serve, in such a time of need, fuel me as I take things day by day. I’m confident in my skills to deliver compassionate care as an EMT, and to exercise my medical education to tackle the challenges that I may face in the wake of the COVID-19 surge.”
Need for Medical Students to Work in Hospitals
New York Governor Andrew Cuomo issued a mandate to increase auxiliary staffing—including medical students—to work in hospitals.
Some medical schools like NYU are letting students graduate early to help out on the front lines. This is another reason Mr. Sharza believed it necessary for students from U.S. and Caribbean medical schools to help out on the front lines.
“I first heard about this a few days into being home,” he said. “The situation in NY was growing worse and worse each day. The Governor of NY ordered hospitals across the state to increase by 50% in preparation for systems to be overwhelmed by the surge of affected patients. Along with this message, he indicated that medical students would be called on to act as auxiliary staff in an ‘on-call’ manner. There was a survey conducted by the NYS Department of Health to Schools of Public Health/Medicine/Nursing which had a statement, “In the event that the novel coronavirus crisis worsens, we need to be creative in finding back-up assistance and the help of qualified medical professionals to supplement our state public health system’s capacity to treat seriously ill coronavirus patients including those that may need to be hospitalized and intubated.”
“Multiple schools down closer to New York City (which is the current hotspot for COVID-19 in NY) are fast-tracking their 4th-year medical students in order to assist hospitals with overwhelmed staff, either via early graduation or serving as unpaid interns. Other initiatives are coming more from individual hospitals which are seeking 3rd and 4th year medical students to help fill empty spots in their current staffing at entry level jobs, such as patient care techs. These are super important positions that need to be filled to help prevent hospital staff and systems, in general, be overwhelmed by acutely ill patients. By allowing 3rd/4th year medical students to become incorporated directly in hospitals on a volunteer basis may provide significant aid to the burden on current healthcare workers that currently exists in hotspots like NYC, but also throughout the state as the situation continues to grow. In any case, we had best be prepared for the worst-case scenario.
“I know that in Massachusetts, both UMASS and Tufts University have implemented fast-tracking, similar to NYU Grossman School of Medicine and Albert Einstein College of Medicine in NY. I’d be willing to bet that this strategy is going to find great success and may be adopted by other states as well. I also have a friend over in the United Kingdom who described a very similar process for their senior medical students.
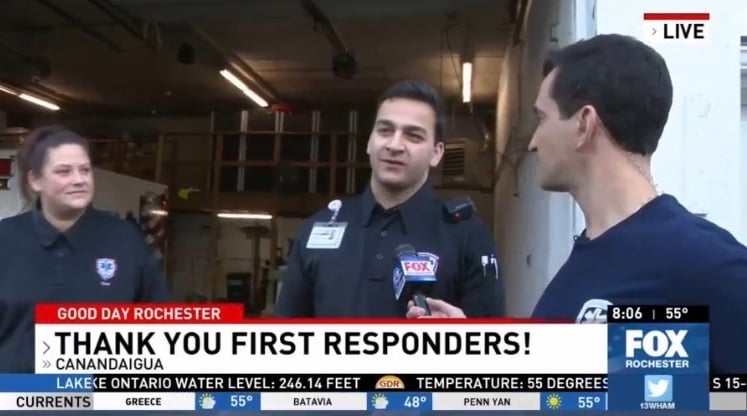
Jared Sharza being interviewed for a local TV news program about roles as an EMS worker & everyday operations. Photo: Courtesy of Jared Sharza.
Med Students & Suspended Clinical Rotations
Why does Mr. Sharza think some hospitals don’t want med students doing clinical rotations now?
“I discussed the topic with one of our Infectious Disease doctors the week prior to suspending clinical rotations,” he said. “He was telling me that the concern would eventually be that the hospital would start to run short on PPE (Personal Protective Equipment) like gloves and masks. During the week prior to asking medical students to leave, the hospital had limited the number of visitors to one per patient at a time in an attempt to further decrease exposure. So, I think that the hospitals, much like the nation, are trying to limit the workers to essential personnel only right now, in order to preserve PPE supplies to last as long as they can. Beyond that, it’s a safety concern to have students who are there only for educational experience at this time. However, much like I described earlier, there are other students who feel as if this is our fight as much as it is everyone else in the medical field. There’s a sense of duty, in that we’ve dedicated so much time and energy to our studies, that risks are acknowledged. I believe that the clinical medical students are going to come up with creative alternatives as we re-shape our roles in order to remain active participants of the medical community.
What about the possibility of doing clinical rotations online?
“I haven’t heard much in terms of from an official plan via announcement or article. I think this has probably stemmed from the majority of basic science programs having transitioned over to online learning platforms. I’d be shocked to think that there is serious consideration in finding value of doing clinical experiences online. 3rd and 4th year of medical school are supposed to be most valued because of the direct patient contact and the art of performing physical exams on our own. That being said, I definitely think education has to continue for clinical students and that all options should be considered for temporary bridges to our clinical rotations.”
Mr. Sharza wants to share how he attempted to become involved at his local hospital.
“Instead of registering for the state list of medical students who would be available per ‘on-call’ basis, should the situation continue to deteriorate, I went directly to my local hospital and inquired directly,” he said. “This is a hospital where my parents have worked through and our primary hospital that we transport patients to for EMS. I shadowed in the Emergency Department in 2015. I’ve become close acquaintances with a lot of the staff in there- from patient care techs, security, nurses and some of the physicians that all work in the ED. It was a no-brainer to me that I check directly with them to see if I could be of help to them since it’s in my own backyard.
“ I contacted our EMS medical director who quickly forwarded my inquiry to the appropriate decision-makers, all of whom welcomed the opportunity to have me come aboard as help should the need arise for the hospital. I was directed to the human resources department and to discuss with them the situation and see if they would have any suggestions on how to move forward. After speaking with the same staff member who had helped me set-up my shadowing experience in 2015, I was informed that I would need to apply for a paid position so that I would be covered in terms of liability. The hospital worked quickly toward fast-tracking me as an employee in a tech title but to be promoted to medical student assignment when the time of need comes. There’s a lot of confusion on exactly what my role with the hospital will entail, largely because the hospital yields that it is uncharted territory for them. My idea of what role I’d play is somewhere similar to the role I had on my rotations- where I’d see a few patients, take history and perform physical exams and then do necessary chart work prior to rounding with my attending. I think that this could help unburden currently active physicians attend to higher priority patients, especially in the ED setting. I have currently been hired as a patient care tech but am in the hospital’s labor pool as a medical student, so when the need arises, I will be promoted from tech work to medical student assignments. In the meanwhile, I will continue to work primarily with EMS.”
 Jared Sharza about to enter the hospital to start a shift. Photo: Courtesy of Jared Sharza.
Jared Sharza about to enter the hospital to start a shift. Photo: Courtesy of Jared Sharza.
6 Ways Med Students Can Help Fight COVID-19
Mr. Sharza outlined many ways 3rd and 4th-year medical students on the front lines can help out local communities in medical capacities.
“There are a lot of articles starting to come out highlighting the response of medical students being ‘sidelined.’ I think that we, as current medical students, will eventually be asked in future interviews-, ‘What did you do during the time that your clinical rotations were suspended?’ I think this is where we can take advantage of an unfortunate opportunity and show our communities that, no, we may not be doctors in the hospital, but we can still be of great service to our communities. I think that by demonstrating initiative and desire to contribute to the frontlines of healthcare, either directly or indirectly, will go a long way not just towards positively impacting our current fight, but also towards proving our worth as the next line of future physicians. Yes, it’s frustrating and irritating that our long journey is on pause, but that doesn’t mean our desire to serve in a medical capacity has to be as well."
Mr. Sharza gave a list of a few alternatives he has read that medical students are engaging in:
1) Collecting/finding donations of PPE from small local businesses and private stocks to supply them to hospitals, EMS, fire departments, police departments. These men and women stand at the very front of the frontline and deserve all the equipment they need. Their concern has to continue to be on patient health, not on whether they’ll be able to safely do their job.
2) Contact your local hospital’s HR department/recruiter and share your status as a medical student and see what options they may have available for you to help out with.
3) Assisting COVID-19 call centers. Most county departments of health have established call centers that they use to monitor and report the state of COVID-19 patients who are self-quarantined. I’ve read that this is a pretty popular form of helping out, albeit indirect. I can see how this would be a great opportunity to practice verbal communication with patients and deriving histories and finding out more about the disease from the patients themselves.
4) Helping hospitals screen incoming visitors for high-risk assessments. This is essential to a lot of hospitals and nursing/rehab homes. Since I’ve been home working with EMS, there is a legitimate need by these places to ensure that those who are coming into their building are not sick or at high-risk of spreading the virus inside of their places. As it stands, especially at the hospitals, they have either nurses or patient care techs at the doors doing these jobs. These are essential employees who would probably be better utilized in the hospital at their own posts. This is something very simple that a medical student could do by asking, “Have you had a fever, shortness of breath, cough recently? Any exposure or contact to anybody sick? Any travel outside the US recently to China, Iran, Italy?”
4) Offering to babysit, animal-sit, or just run general errands to current hospital workers. This is something you could just send an email out to a hospital or give them a call and see if you they could advertise your voluntary support with these things. Again, this is one of those things that could and should help keep the priorities on the patients and not worrying about life outside of the hospital.
5) Become educated on the matter, and then educate (FYI- the word “doctor” in Latin stems from the verb docere, meaning- to teach). Coronavirus is a three-minute video on sketchy-micro (probably in need of an update), but the current novel virus is having significant complications requiring intensive ventilator management. As medical students, we know that pathology and physiology are all at the backdrop of these significant complication as it is notoriously causing Acute Respiratory Distress Syndrome (ARDS). Now, more than ever, would be a great time to brush-up on the topic and the pulmonary pathophysiology involved so that we can confidently address questions on the subject (like the next time your friend or family member texts/calls you wanting juicy details). Research what the current guidelines are according to the CDC, and also go to your own state’s Department of Health website and see what initiatives are going on.
6) Be creative, inspired, and ever motivated by your fellow medical students. Engage in dialogue with other medical students at different schools and see what they’re doing to impact their communities.
 Jared Sharza at the end of a long shift in the ICU. Photo: Courtesy of Jared Sharza.
Jared Sharza at the end of a long shift in the ICU. Photo: Courtesy of Jared Sharza.
Doctors Mr. Sharza has worked with recently say current medical students will be defined by what they do now. What does that mean to him?
“When I started to hear doctors talking about this, it re-affirmed my decision to come home and get right back to work with EMS. At the time I decided to come home, I wasn’t thinking- what can I do during this time to boost my future credentials; I just knew that I had to come home because there were a lot of people suffering and a lot more people were going to be effected soon enough. But this is definitely a talking point for current medical students displaced from their clinical rotations in the future during interviews, ‘What did you do during your time off from clinical rotations?’ I’ll be proud to say that I stepped up without hesitation, as I felt it was my duty to help in a capacity that I was comfortable with and had experience in (EMS)."
He has strong words for younger people under 40 who still aren’t taking the pandemic seriously and are not practicing social distancing.
“When COVID-19 first started to come around, I was pretty ambivalent about it,” he said.” I didn’t realize the ultimate impact it would have on social, political, or economic lives. Once I started to notice the precautions that were taking shape in my community, I started to pay attention more. It wasn’t until I was home and working in EMS when I would start to see the immediate impact that COVID-19 can have. I was hearing more and more horror stories from nurses and residents down in New York City, I read more articles, and started to monitor the data about the disease. I think that we had an early flaw in presumption that COVID-19 would only severely impact our elder population. I think that this was an interpretation that many people came away with after the first few weeks with the virus in the USA. Now that we’re starting to see that this disease is affecting a broad spectrum of people— both with and without underlying diseases— I think we’re gravitating towards more respect towards the practice of general precautions, including social distancing. We can do better by emphasizing to our younger population that there most definitely are consequences that exist and are threatening us from the shadows. No, young adults with relatively healthy immune-systems may not be as severely impacted with the disease, but the reality is that we are constantly transmitting germs both from our respiratory secretions in the air and also through physical contact and those who are silently effected by this virus may be contaminating every day utensils that can eventually expose someone else down the line. So, in essence, I’d feel compelled to further explain this process of transmission to young people who are not respecting social distancing, because they may not be aware of the details and instead are only fixated on being at lower-risk than other populations.”
How would he describe what’s going on at the hospitals that he has seen firsthand?
“Since the majority of my time during this COVID-19 surge has been with EMS, I can only speak on behalf of what I’ve seen and what the guidelines are. Hospitals are sectioning off areas of their floors for COVID-19 patients only and creating separate entrances with dedicated staff as to limit exposure. There is a main concern for severely ill patients who require advanced airway support via the use of ventilators and hospitals are trying to aggregate their resources and staffing as well. Because of the prevalence and novelty of this virus, there is a high-index of suspicion as soon as these patients enter the hospitals until ruled out with questioning and basic vitals (if they’re symptomatic, that is).”
Has he personally had to work with any COVID-19 patients, either positive or suspected to be positive? And what kind of protective precautions is he taking?
“I went on one call (so far) in EMS where we were dispatched for respiratory distress with coughing and were cautioned that the patient had tested positive 10 days prior for COVID-19,” Mr. Sharza said. “When we arrived at the address, the wife came out and she was wearing a mask and was explaining what was going on. 10 days ago, the patient had returned from New York City after becoming sick and subsequently tested positive for COVID-19 and was recommended to be placed on quarantine with his wife as well. Six days after that he progressively got worse and was prescribed antibiotics to go home with. He continued to decline until his presentation for the emergency call. My partner and I returned to our ambulance and gowned up in the appropriate N-95 mask, double gloves, protective glasses, and isolation gowns. On calls of this nature, we also have first responders and firefighters come to the scenes as well. Because this was a known positive patient, we decided to have the other first responders stay outside as to limit the exposure. We gave a mask and pair of our gloves to the patient’s wife so that she could have him put them on. The idea behind this was to make it so that we could exercise droplet as well as contact precaution on his behalf as well. When we entered the house, the patient’s wife indicated that he was upstairs in his room sitting in a chair. When we got to him, he was in moderate respiratory distress and we could assess from the scene that he had some sort of respiratory disease and diabetes (glucometer and CPAP on his side of the bed). His cough was concerning and we decided we needed to get him started on high-flow oxygen in the ambulance. We followed our COVID-19 EMS guideline and called our local hospital who informed us that the patient would have to be transported to a higher level of care facility instead. After treatment with oxygen only, the patient’s cough subsided and he indicated that he was feeling better. After getting him transported, safely and without further complaint, we returned to our ambulance, took off all of the blankets and covers (like we always do after every call), and decontaminate it with CaviWipes. After our stretcher was cleaned, we had to decontaminate the whole patient compartment of the ambulance with the CaviWipes. Since my partner and I had direct patient contact with a COVID+ patient, we now have to wear surgical facemasks as a precautionary measure for 14 days and monitor for signs/symptoms every 12 hours.”
There had been talk by politicians about possibly opening the nation back up by Easter, but now the date has been pushed up to April 30. Does anything about opening the country back up and easing up lockdown restrictions early make any sense from a scientific or political perspective?
“With the daily increase in numbers of confirmed cases in the US across each state, I’m hard-pressed to believe that this is going to slow down in the near future,” he said. “In fact, I think that we have yet to see the worst day in terms of morbidity and mortality of COVID-19. Having read many articles, analysts predict a 14 to 21-day timeline before reaching an apex of cases. With Easter falling sometime during that estimation, it would be a public health nightmare. I understand that Easter is a time of coming together for many people in different social settings. I think the realization that this is going to get more severe and impactful as we continue on this timeline. I’d press for awareness and patience during this time. I’m also understanding that time is money for everyone, especially those most impacted financially by the virus; but even still, you can’t place a price tag on human life. We can and will rebuild and recover from this international crisis, but it will take time.”
What else does Mr. Sharza think med students on the front lines need to know now?
“For any professional student in health-related fields whose journey is on pause, I implore you to not burden yourself with frustration and self-pity,” he said. “I understand the time, energy and spirit we are all putting towards our goal and I understand your emotions. We can’t dwell on what we can’t change, but we can take action and positively impact those around us using skills and practices we’ve come to learn along the way.”
The UMHS Endeavour and UMHS website will be updated regularly as news of the pandemic unfolds.
If you would like to be interviewed in the UMHS Endeavour as either UMHS alumni or one of our students on the front lines, please email Scott at sharrah@umhs-sk.net
(Top photo) UMHS student Jared Sharza returned to work as an EMS worker in Upstate NY after his clinical rotations in Detroit were temporarily suspended due to COVID-19. Photo: Courtesy of Jared Sharza.
About UMHS:
Built in the tradition of the best U.S. universities, the University of Medicine and Health Sciences focuses on individual student attention, maintaining small class sizes and recruiting high-quality faculty. We call this unique approach, “personalized medical education,” and it’s what has led to our unprecedented 96% student retention rate, and outstanding residency placements across the USA and Canada. UMHS is challenging everything you thought you knew about Caribbean medical schools.

Scott is Director of Digital Content & Alumni Communications Liaison at UMHS and editor of the UMHS Endeavour blog. When he's not writing about UMHS students, faculty, events, public health, alumni and UMHS research, he writes and edits Broadway theater reviews for a website he publishes in New York City, StageZine.com.