The media and public health experts have discussed a “second wave” of COVID-19 in the fall of 2020 and winter 2021, but UMHS alumni working on the front lines of the pandemic and UMHS faculty—like many healthcare experts—have different perspectives on what a “second wave” means, and some feel we are still in the first wave or even one continuous wave. Top epidemiologists are warning that the worst of the pandemic is ahead in the next three months.
The UMHS Endeavour spoke to four UMHS alumni on the front lines and two faculty members about the COVID-19 “second wave” in the US and why doctors and healthcare professionals may now be better prepared to treat patients with new therapeutic medications and better knowledge of how the novel coronavirus affects the body. We spoke to doctors and faculty about other factors such as treating patients who have COVID-19 denial and think it is a hoax, why flu shots are especially important this year, mental health advice for front-line workers, plus general tips and guidelines for med students and doctors on how to cope with COVID-19 and treat patients during this challenging time.
 Dr. Alex Zayid in PPE while working a shift at Ascension Providence Hospital in Michigan. Photo: Courtesy of Dr. Zayid.
Dr. Alex Zayid in PPE while working a shift at Ascension Providence Hospital in Michigan. Photo: Courtesy of Dr. Zayid.
Are We Really in a ‘Second Wave’ of COVID-19?
In the United States, COVID-19 cases continue to rise in most states as the weather gets colder and people have started moving indoors, where transmission is more likely to occur. The number of deaths has risen to more than 220,000, 14 states have reached hospitalization records, and daily coronavirus case numbers are at levels the USA has not seen since the summer, CNN reported.
A record 83,000 new COVID-19 cases were reported on Friday, October 23, 2020, “more than 6,000 higher than the country's previous record set in July.”
COVID-19 hospitalizations set records in 13 states this week, Dr. Anthony Fauci told CNBC's Shepherd Smith on Wednesday, October 28, 2020.
"If things do not change, if they continue on the course we’re on, there’s gonna be a whole lot of pain in this country with regard to additional cases and hospitalizations, and deaths," Dr. Fauci said,
NBC News reported that the United States recorded a record 90,000 COVID-19 cases in one day for the first time ever on Thursday, October 29, 2020.
Public health officials have warned that the United States may see the worst of the pandemic in the next six to 12 weeks. The UMHS Endeavour spoke to several front-line doctors, most of whom said they believed it was difficult to declare the USA as being in a “second wave” because the data is, so far, different in each region, but some epidemiologists warn that the USA might even see a “third wave” later this winter.
 (Inset, right) : Dr Alex Zayid, UMHS 2019 grad, is working on the front lines at a Michigan hospital. Photo: Courtesy of Dr. Zayid.
(Inset, right) : Dr Alex Zayid, UMHS 2019 grad, is working on the front lines at a Michigan hospital. Photo: Courtesy of Dr. Zayid.
Dr. Alex Zayid, a UMHS 2019 graduate currently working on a Family Medicine residency with a focus on Preventative Medicine at Ascension Providence Hospital in Southfield, Michigan, said he is not sure whether we are technically still in the first wave or second.
“I think it's tough to say whether we are at the tail end of the first wave or the very beginning of our second wave,” he said. “Throughout the country we experienced many different regions get hit at different times with varying severities. That being said, we are entering flu season. I think the numbers in the coming months will answer this question for us.”
 (Inset, right) : Dr. Jordan Stav, UMHS 2018 grad & Emergency Medicine resident at a Michigan hosptial. Photo: Courtesy of Dr. Stav.
(Inset, right) : Dr. Jordan Stav, UMHS 2018 grad & Emergency Medicine resident at a Michigan hosptial. Photo: Courtesy of Dr. Stav.
Dr. Jordan Stav, UMHS 2018 grad, is an Emergency Medicine resident at Ascension Macomb-Oakland Hospital in Michigan and has similar sentiments.
“It’s really hard to say, due to every region, state and municipality handling the pandemic differently; it hit the entire country in different ways at different speeds,” Dr. Stav said. “In Michigan, we were hit hard at the beginning and then due to lockdown dropped in cases dramatically. Now, we are seeing cases trickle into the emergency departments—nothing like we saw in March and April—but still present. It is hard to say if this is still a downslope or back on the uptick. I'll leave it up to the public health officials to determine where we are on the charts. More importantly, COVID-19 is here to stay for the foreseeable future and always in our minds while evaluating patients.”
 (Inset, right): UMHS grad Dr. Melissa Alvarez in PPE on a shift at Mercy Catholic Medical Center in Pennsylvania. Photo: Courtesy of Dr. Alvarez.
(Inset, right): UMHS grad Dr. Melissa Alvarez in PPE on a shift at Mercy Catholic Medical Center in Pennsylvania. Photo: Courtesy of Dr. Alvarez.
UMHS 2017 graduate Dr. Melissa Alvarez, Internal Medicine resident PGY-III at Mercy Catholic Medical Center in Darby, Pennsylvania also said the first or second wave depends on the geographic region of the US.
“If we are talking about the USA as a whole, then I feel like we are still in the first wave,” she said. “If you look at our numbers, we are waving up and down. We’ve never achieved a long-term plateau. If you look at the country regionally then there are areas that I would say are out of the first wave. The Northeast would be an example of a region that got their numbers under control and are now starting to see a rise upwards again. There are also some regions where they are just getting their first big spike. So, I would say regionally some places are starting to see a trend towards a ‘second wave’ but as a country we are in the same wave we’ve been in.”
 (Inset, right): Dr. Rahul Gossain, UMHS grad & Hematology & Oncology physician at the Guthrie Corning Cancer Center in Corning, NY.
(Inset, right): Dr. Rahul Gossain, UMHS grad & Hematology & Oncology physician at the Guthrie Corning Cancer Center in Corning, NY.
Dr. Rahul Gosain, a UMHS 2012 graduate, Hematology & Oncology physician at the Guthrie Corning Cancer Center in Corning, New York, and MBA candidate in Healthcare at the Johns Hopkins Carey School of Business, also said the issue of being in a first or second COVID-19 wave is based on the regions of the USA.
“In some parts of the country, we are still in the first wave as we battle active outbreaks and yet to see a plateau,” Dr. Gosain said. “Whereas, in other parts of the country such as New Jersey and New York City, we are seeing the early phase of the ‘second wave’. The pandemic has affected different regions of the country in different ways over the last 10 months. Some states and cities saw an early severe outbreak and then a down-trend, whereas, in other parts of the country, the numbers are still surging up.”
Whether we are still in the first or second wave of COVID-19 is “somewhat semantic,” said Edwin S. Purcell, Ph.D., UMHS Associate Dean of Academic Affairs.
 (Inset, right): Dr. Edwin Purcell, UMHS Associate Dean of Academic Affairs. Photo: Courtesy of Dr. Purcell.
(Inset, right): Dr. Edwin Purcell, UMHS Associate Dean of Academic Affairs. Photo: Courtesy of Dr. Purcell.
“There was one peak, cases went down and there was another (larger) peak,” Dr. Purcell said. “Some would call it a second wave since cases have risen again, while others feel that the dip after the first wave was not sufficiently low to say the first wave had ended. The second is Dr. Anthony Fauci’s opinion, which I greatly respect.
Are We Better Prepared to Treat COVID-19 Now?
When COVID-19 first started wreaking havoc in the United States back in March, hospital emergency rooms and ICUs were overwhelmed. There were few proven therapeutic treatments, and many critically ill patients with shortness of breath were put on ventilators. Seven months later, are doctors and healthcare providers better prepared to treat patients?
Dr. Alex Zayid said he believes the American healthcare system has made some progress in treating COVID-19 because we are now no longer blindsided by the novel coronavirus.
“During the first wave, we did not know if this virus was in the States, let alone how to treat it,” he said. “By the time we had cases here, it was too late and had already been spread to a point that hospitals could not catch up. It was a learning process for the entire health system; this time around we not only have a tested approach to treating COVID-19, but our hospitals have systems in place to be proactive towards the virus rather than reacting out of panic.”
Dr. Stav said that while we know much more about COVID-19 and treatment and have made progress, many unanswered questions remain.
“We have more PPE, we are quicker to use steroids in those with respiratory compromise, we are more cautious with unfounded and unproven methods of treatment,” he said. “We are also trying to keep people off of the ventilators for as long as possible, but sometimes it is inevitable. We still don't know many things though; such as who will have untoward effects months after initial infection and what those reactions may be.”
Dr. Alvarez said doctors are certainly more prepared now than last spring.
“We know a little bit more about the disease course and what to expect,” she said. “We have medications like Decadron (a steroid which has been shown to reduce mortality) and Remdesivir (an antiviral which has been shown to reduce time to recovery) that have been useful. We don’t have a cure, but I think we have actual treatment plans now and we don’t feel as lost when treating COVID-19 patients.”
Dr. Gosain said that even after the first reported case in the world in fall 2019, little is still known about the SARS-Co-V-2, the coronavirus that causes COVID-19.
“However, we have made some progress,” he said. “We now know that this virus is very contagious and universal masking, along with social distancing and good hand hygiene, could slow the spread. No one particular treatment or medication has been shown to eradicate the virus but recent data support the use of steroids in high-risk situations to suppress the cytokine/immune response and help the patients in their recovery. Furthermore, hospitals have more PPE for their front-line healthcare workers. However, we will be facing new challenges as we collide with the flu season along with the ongoing pandemic”
Dr. Purcell of UMHS said that the American medical community has made many advances in treating COVID-19 patients. For starters, the death rate has decreased from “around 5% to slightly less than 3%.” However, the death rate may increase if the pandemic curve goes up as winter approaches.
Last spring, critically ill COVID-19 patients were often put on ventilators, but that has changed now.
“More effort is put into keeping people off ventilators and if a ventilator becomes necessary, patients are placed in a prone position,” Dr. Purcell said. “In some instances, extracorporeal oxygenation is available which can alleviate the need for ventilators. Convalescent plasma and Remdesivir can modestly shorten the time of hospitalization. Dexamethasone [a corticosteroid for the lungs] has been a bit of a game changer in preventing the cytokine storm which causes much of the damage in severe cases.”
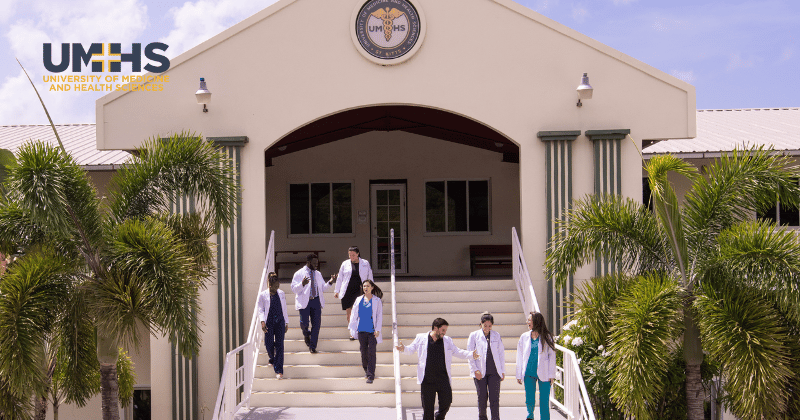
Discover if a Caribbean Medical School is right for you.
Learn about the most popular alternative path to becoming a doctor.
Are Hospitals Now Better Prepared for COVID-19?
Dr. Zayid said his hospital in Michigan is taking all the necessary precautions.
“We continue to screen at every door for temperature, symptoms and contact with sick patients. We insist that employees remain home if they are symptomatic and get tested to ensure to safety of all of their peers and patients.”
Dr. Alvarez said Mercy Catholic Medical Center in Pennsylvania has made many adjustments, and she has had to adapt to the ever-changing environment in the hospital.
“When we were in our [first] COVID-19 surge and were to the point where we had to create a second ICU, we were only allowing one person on the team to round on the patient so we could conserve PPE and avoid exposure,” she said. “We tried to group our medication and lab orders to be at the same time to reduce the amount of times the nurses were entering the room. There were some changes to how many people should be in the room in a Code Blue situation. Personally, I have a bag that I bring to work with me that has hand sanitizer, moisturizer, and Lysol spray. I see every patient with an N95 face mask, and gloves. My program has had most of our teaching converted to virtual lectures so we aren’t all in the same conference room and a lot of the events we normally have been cancelled or changed to virtual (for example, the Class of 2020 had a virtual graduation).”
Dr. Jordan Stav said his Michigan hospital follows simple new rules.
“While with your patient, you don't have the luxury of distancing. So, wear a mask, wear gloves, wash your hands and stethoscope after every encounter.”
How Keeping Track of Public Health Data Can Save Lives
Coping with COVID-19 and treating patients, contract tracing and helping the public mitigate risk are all dependent on the most up-to-date public health data.
It is imperative for healthcare professionals to monitor epidemiological statistics regularly, said Dr. Rahul Gosain.
“Following the trends and the data in regards to the spread is of the essence so that patients traveling from high-risk areas can quarantine adequately to keep the community and their loved ones safe, he said. “During the early days of the pandemic, the phrase ‘flatten the curve’ gained a lot of traction—this concept is still very important as we anticipate the convergence of COVID surge and flu to overwhelm our hospital systems. Taking care of 500 patients in a community in one day versus serving the same number of patients over a week or two will result in completely different outcomes. Since the origin of the infection, we do believe that the virus has evolved and new strains have merged, but there is thought to be little variability between these strains. However, the first case of re-infection in the United States was recently reported and there is yet a lot to learn from this new finding.”
Dr. Melissa Alvarez said there are two key factors to consider regarding the data.
“The two most important numbers, in my opinion, are the test positivity rate and the daily hospitalizations,” she said. “People say that we are finding more cases because we are testing more. While we are testing more than we were in the beginning of the pandemic, more testing alone will not cause a rise in cases. This is why the test positivity rate is important; this number tells you what percentage of the tests conducted that day were positive results. If we are getting control of the spread, the positivity rate should be below 5%. If an area is above 5% positivity, that area is at risk for a more large-scale outbreak. This positivity number can also help you determine your own personal risk when you’re considering doing certain activities. If in your area, the positivity rate is 2% it is likely less of a risk for you to go eat at a restaurant or have a small get together with a couple of friends than if the positivity rate is 8%.
Daily hospitalization trends are also crucial.
“This number is especially important as we hit the winter months, when hospitals usually experience a higher census,” Dr. Alvarez said. “The important thing isn’t just the daily numbers, but what the trend looks like. Have hospitalizations been climbing steadily for the last week? If so, that’s likely a sign that community spread in the area is increasing. It is also a sign to the hospitals that they need to get ready for a higher census than a normal winter season. If hospitalizations have been steadily declining, that is likely a sign that community spread is lower.”
Dr. Alex Zayid in Michigan concurred.
“If we learned anything throughout the first wave COVID-19, it is that trends are real with the spread of this virus,” he said. “Michigan was hit earlier than other regions of the country which triggered more aggressive regulations out of our government luckily yielding a great response to the virus. Information like this should be widespread throughout the country for other regions to see how different measures work, how the virus is spreading and hopefully predict spikes in other areas.”
Dr. Edwin Purcell of UMHS said it is vital to follow all federal, state and local guidelines and mandates as they are designed to save lives.
“Keeping track of the new daily cases in your state and in your county keeps you in touch with how well mitigation efforts are working,” he said. “Test positivity rates give a reflection of total spread in the community but they also give insight into how adequate testing measures are. If testing is limited only to those who show symptoms, the percentage testing positive will be high (8% or more). That also means it is likely that there are many asymptomatic cases that can be spreading the disease. Rates below 5% mean there is sufficient testing to find those asymptomatic individuals and have them quarantine to stop the spread. Obviously, hospitalizations and deaths give you an idea of the impact of COVID-19. In particular, I think ICU capacity is an important figure to pay attention to. The worst-case scenario is that there are so many cases that the hospitals literally cannot properly handle the number of critical patients. We all play a role in ensuring this does not happen. To eradicate the disease, it is important that we identify people who have been exposed so they can avoid spreading it to others. In many local areas, contact tracing is insufficient to prevent the spread of infection.
"At least six different strains of COVID-19 have been identified, but the overall mutation rate is low. The low mutation rate increases the probability that a vaccine will remain effective for a more extended period of time.”
How Should You Treat Patients with Covid Denial?
The public has different feelings about COVID-19 for a number of reasons both politically and economically. So, what should med students, doctors and healthcare professionals do when a patient says COVID-19 won’t affect them or is a hoax?
Dr. Alex Zayid said to avoid arguing when a patient has COVID-19 denial.
“There is a lot of distrust in the medical community today, I do not blame patients; you should not either,” he said. “Do not get defensive, rather try to understand why they think this way. For many people, they have resentment towards COVID-19; it took some of their jobs, their homes, their plans. Help these patients to understand that, although it has not affected their personal health, we are stronger as a unified community getting through this together.
Dr. Tess Maguire, a faculty member at the UMHS campus in South Portland, Maine, stresses empathy when one encounters a patient with COVID-19 denial.
 (Inset, right): UMHS faculty member Dr. Tess Maguire. Photo: Courtesy of Dr. Maguire.
(Inset, right): UMHS faculty member Dr. Tess Maguire. Photo: Courtesy of Dr. Maguire.
“Be patient,” Dr. Maguire said. “When you meet someone with ideas different from your own, listen, understand where they are coming from and put yourself in their shoes. Even before you get to that point, you have to be ready and equip yourself with the knowledge about COVID-19 as with other diseases and you will have more certainty and conviction. As it is, there is still much to learn about this illness and it is necessary to keep up with up-to-date information as we move on. If you encounter people who are in denial about COVID-19, just speak with them sincerely and if still they do not believe, realize that you would have done your best and that is all you can expect of yourself, nothing more. You may not know that, in speaking with you, receiving your care and attention, change may happen.”
The ever-changing scientific data about the virus can be confusing to doctors and patients alike, Dr. Gosain said.
“As we learn more about this virus, the recommendations will continue to evolve and it is understandable for us to expect some frustration from the patients as what we recommend will change. But, educating patients and showing the data behind current recommendations: social distancing, universal masking, and good hand hygiene are the key.”
Sometimes even critically ill COVID-19 patients refuse to accept the fact that the virus is real. What should one do in this situation?
“My advice would be to ignore it,” said Dr. Edwin Purcell of UMHS. “There are patients who have died from COVID-19 who refused to admit it was real.”
 UMHS front-line alumni doctors & faculty members all agree flu shots are especially important during the COVID-19 2nd wave because the two illnesses have similar symptoms. Photo: Deposit Photos.
UMHS front-line alumni doctors & faculty members all agree flu shots are especially important during the COVID-19 2nd wave because the two illnesses have similar symptoms. Photo: Deposit Photos.
Why Are Flu Shots so Important in the Fight Against COVID-19?
Each fall, doctors recommend flu shots to help protect patients from severe influenza. Even before COVID-19, many people have refused to get an annual flu vaccine for a variety of reasons, but because flu and COVID-19 often have similar early symptoms (such as a high fever), public health experts have advised everyone to get a flu shot this year.
Dr. Jordan Stav in Michigan agrees that flu shots are vital and necessary for the 2020-2021 flu season.
“This has always been emphasized; regardless of COVID-19,” Dr. Stav said. “Flu vaccine does not guarantee you will not get the flu; in fact, it often does not protect against this year's flu. It's a guessing game from year to year. However, it has been proven to decrease the severity of infections. It is also theorized that if you get flu immunizations throughout your lifetime, there will be an additive effect of protectiveness. This year, it obviously matters because if it turns out to be a bad flu season on top of a COVID-19 resurgence, I can't imagine having both at the same time. Let alone passing it along to family or friends.”
Dr. Edwin Purcell has similar thoughts.
“There is real concern that a bad flu season combined with COVID-19 could overwhelm our healthcare systems. Flu shots are not a guarantee that you won’t get the flu. Scientists have to guess a year in advance which will be the most prominent strains of flu. That said, it can decrease the likelihood of getting the flu and spreading it to others. If you do still get the flu, it is likely that it will be milder and shorter in duration.”
Dr. Melissa Alvarez in Pennsylvania said she is a big advocate for flu shots and she always reminds patients, friends and family to get vaccinated.
“This year will be more important than ever to get as many people vaccinated as possible,” she said. “Early is better because it takes some time for your body to get the full effects of the vaccine, so you want to make sure to get it before the flu starts to have wide community spread in your area. Yes, the vaccine is not 100% effective at preventing flu. However, it has been shown to reduce the need for hospitalization from the flu and that is extremely important this winter season. It will be extremely burdensome to our healthcare system to have large hospitalization numbers from two different viruses at once. Please get vaccinated; I’ve already had mine.”
Dr. Rahul Gosain also said he believes getting a flu shot early is crucial this year.
“As we embrace the annual flu season, getting a flu vaccine as soon as possible this year is more important than ever. Though this vaccine will not protect us against SARS-CoV-2, historically flu vaccine has ‘shown to reduce the risk of flu illness, hospitalization, and death’ as stated by the CDC. This will help the patients to stay out of the hospital which will indeed decrease their risk of getting exposed to COVID-19 but also give a chance for healthcare systems to use their resources for the care of patients with COVID-19.”
Dr. Tess Maguire of UMHS said she agrees with the recommendation of getting a flu shot annually to protect against influenza and, as other doctors have said, the 2020/2021 is especially high risk.
“This flu season in particular, because many of the signs and symptoms of Covid-19 are similar to the flu, like fever, chills, body aches, fatigue, cough, sore throat, runny or stuffy nose, headache, it is important to have this protection,” Dr. Maguire said. “If the vaccinated individual comes down with any of these symptoms, at least it would be less likely that it is from the flu, although remember that there is still a possibility because even the vaccine does not give 100 percent protection as it can depend on the strain of circulating influenza when it happens. The good news is that being both respiratory viruses, the physical measures to help prevent both infections are the same.”
Mental Health Advice for Front-Line Healthcare Workers
There are many mental health issues related to the pandemic. Two front-line doctors interviewed discussed ways that doctors, med students and the public can ease their anxiety and depression about dealing with so many sick people, patients dying, and grappling with isolation and quarantine.
Dr. Melissa Alvarez said the mental health aspects of working on the front lines were a huge struggle for her at the beginning of the pandemic.
“I was very worried about becoming infected with COVID-19 and bringing COVID-19 home to family,” she said. “I didn’t visit anyone for about three to four months to avoid spreading the virus and felt grateful that I live alone in my apartment. It was also extremely difficult to feel like you had nothing to offer patients, and dealing with the amount of death that we saw (there was one night that six COVID patients died during our peak surge), and dealing with the emotions of patient families because they couldn’t even visit their dying loved one. It was a lot to handle, and the fact that we were basically just going to work and then going home to sleep really didn’t help matters.”
What should healthcare workers do when they feel overwhelmed?
“The best piece of advice I can give would be to find someone to talk to about what you’re feeling: a friend, a mentor, a therapist, a family member, a coworker,” she said. “I also made sure to try and take time to do something that was important to me, which for me was working out. I would go for a walk or a run or do a workout in my apartment. I did something to help me escape for a bit and just focus on something else. Finding your outlet is important: get lost in music, listen to a podcast, watch Netflix, draw, color, read a book…. something that lets you escape reality for a moment.”
Dr. Alex Zayid said that as healthcare professionals, it is quite easy to get lost in one’s work while forgetting to take care of one’s self.
“Giving back to others is a passion we have each had for as long as we can remember (or you would not have made it this far in this day of medicine),” he said. “That being said, you are no good to your patients if you are not good to yourself. This is advice easier said than done, but remember to focus on your wellness so you can come into work each day as the sharpest, most positive version of yourself to provide the best care possible. I am a huge believer in positivity, both in your personal life and as something that can be exuded to your patients. Stay positive and allow both your patients and colleagues to match your energy on the floor, even in the darkest of times... it will help you all through."
Advice for Med Students Entering Clinical Rotations
Dr. Tess Maguire has several things to say to med students about to enter clinical rotations during the COVID-19 pandemic.
“Know more about COVID-19 and be aware of the updates as they come,” she said. “The more you know about something, the better you can be prepared. Medical students would generally know the physical measures to help prevent this infection such as wearing a face mask, social distancing which is currently recommended to be at six feet, hand sanitizing or handwashing with soap and water for at least 20 seconds which is actually the most important means of helping to prevent nosocomial or hospital-acquired infections, wearing the other appropriate Personal Protective Equipment (PPE) like a face shield or goggles and gloves when seeing patients. When taking care of COVID-19 patients specifically, there will be additional layers of protection like the use of N95 mask and gown. However, it may be that medical students will be assigned to care for patients who are not known or suspected to have COVID-19. Nevertheless, one has to be mindful that up to about 45% of positive cases are asymptomatic. Therefore, we have to remember to always practice the habits that we have learned in the past months that have been mentioned above.”
Dr. Maguire also stressed the need for med students to take care of themselves in order to help keep their immune system strong.
“There are other important basics of self-care such as eating a healthy diet, exercise, getting enough sleep at night and having a hobby to help cope with stress. If you are someone who has faith, then prayers will help. Others resort to music or connecting with loved ones on the phone or social media. In the end, remember that, as you take care of yourself and stay healthy, you are also taking care of all those who are around you. Begin taking good care of yourself now (or some would say, yesterday).”
Dr. Edwin Purcell of UMHS advises students to look to staff, peers and alumni for advice and support.
“First, be sure to follow all instructions from your attending physicians,” he said. “Second, I think we should set up a buddy system so that new clinical students can speak with our students/former students who have been through it.”
(Top image): As cases surge, public health officials warn we the next three months will be critical as we enter the 2nd wave of the COVID-19 pandemic. Image: Deposit Photos.

Scott is Director of Digital Content & Alumni Communications Liaison at UMHS and editor of the UMHS Endeavour blog. When he's not writing about UMHS students, faculty, events, public health, alumni and UMHS research, he writes and edits Broadway theater reviews for a website he publishes in New York City, StageZine.com.